Adriamycin, a potent anti-cancer drug, has revolutionized the treatment of various malignancies. Its discovery marked a significant milestone in cancer therapy, offering hope to countless patients battling life-threatening diseases. This remarkable compound, with its unique chemical structure and potent biological activity, has become a mainstay in the arsenal of oncologists worldwide.
Adriamycin’s mechanism of action involves interfering with the DNA replication process in rapidly dividing cancer cells, effectively halting their growth and proliferation. This targeted approach, coupled with its ability to penetrate cell membranes and reach the nucleus, has made it a highly effective treatment for a wide range of cancers, including leukemia, lymphoma, breast cancer, and many others.
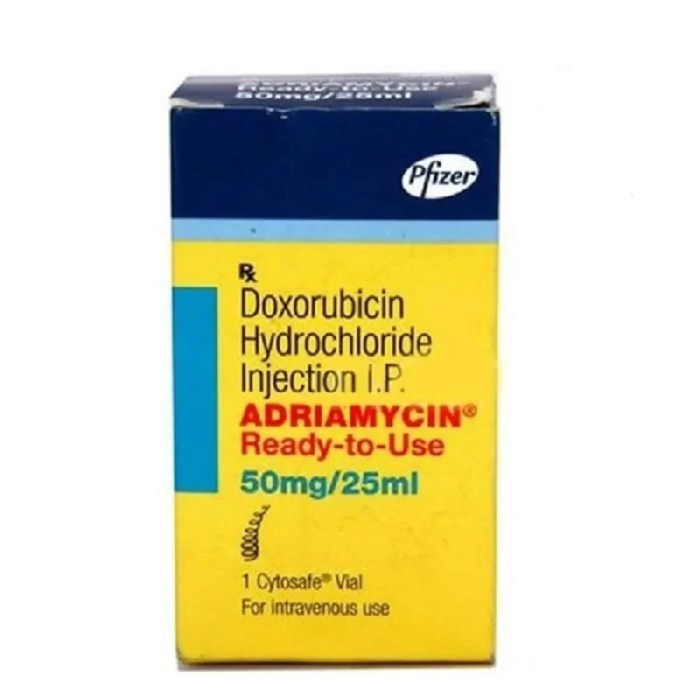
Adriamycin
Adriamycin, also known as doxorubicin, is a potent anti-cancer drug widely used in the treatment of various malignancies. Its effectiveness stems from its ability to interfere with DNA replication and repair, ultimately leading to cell death. This powerful drug has played a crucial role in improving cancer treatment outcomes, making it a cornerstone in modern oncology.
Mechanism of Action
Adriamycin’s effectiveness lies in its ability to disrupt the normal functioning of cancer cells. Its primary mechanism of action involves intercalation into DNA, effectively blocking DNA replication and repair processes. This disruption leads to the accumulation of DNA damage, ultimately triggering cell death through apoptosis.
Adriamycin’s mechanism of action can be further explained through the following steps:
- Intercalation into DNA: Adriamycin’s planar structure allows it to insert itself between the base pairs of DNA, effectively blocking DNA replication and transcription.
- Topoisomerase II Inhibition: Adriamycin also inhibits the activity of topoisomerase II, an enzyme essential for DNA replication and repair. By interfering with this enzyme, Adriamycin further exacerbates DNA damage.
- Free Radical Formation: Adriamycin’s quinone structure allows it to generate free radicals, which can damage DNA and other cellular components, ultimately leading to cell death.
Chemical Structure and Properties
Adriamycin’s unique chemical structure is responsible for its potent anti-cancer activity. Its chemical name is (8S-cis)-10-[(3-amino-2,3,6-trideoxy-α-L-lyxo-hexopyranosyl)oxy]-7,8,9,10-tetrahydro-6,8,11-trihydroxy-8-(hydroxyacetyl)-1-methoxy-5,12-naphthacenedione.
Adriamycin is characterized by the following key structural features:
- Anthracycline Ring: The anthracycline ring is the core structure of Adriamycin and is responsible for its intercalation into DNA.
- Sugar Moiety: The sugar moiety attached to the anthracycline ring is responsible for Adriamycin’s solubility and ability to interact with cellular membranes.
- Amino Sugar: The amino sugar attached to the sugar moiety is responsible for Adriamycin’s ability to interact with DNA.
- Quinone Group: The quinone group is responsible for Adriamycin’s ability to generate free radicals.
Adriamycin’s properties, including its solubility, stability, and ability to interact with DNA, are directly influenced by its chemical structure. Its planar structure facilitates intercalation into DNA, while its sugar moiety enhances its solubility and allows it to penetrate cell membranes.
Historical Development and Discovery
Adriamycin’s discovery and development as a cancer treatment is a testament to scientific progress in the fight against cancer.
The story of Adriamycin began with the discovery of daunorubicin, another anthracycline antibiotic, in the 1960s. Daunorubicin showed promise in treating leukemia, but its effectiveness was limited by its cardiotoxicity. Researchers continued to explore other anthracycline antibiotics, leading to the discovery of Adriamycin in 1969.
Adriamycin was initially tested in animal models and showed remarkable anti-cancer activity. Clinical trials in humans began in the 1970s, and the results were promising. Adriamycin was approved for use in the United States in 1974 and quickly became a standard treatment for various cancers.
Since its discovery, Adriamycin has been extensively studied, and its use has been refined to maximize its effectiveness and minimize its side effects. This ongoing research has led to the development of new formulations and strategies for administering Adriamycin, improving its therapeutic index.
Clinical Applications of Adriamycin
Adriamycin, also known as doxorubicin, is a potent chemotherapy drug that has been widely used in the treatment of various cancers since its introduction in the 1970s. Its effectiveness against a broad spectrum of malignancies has made it a mainstay in cancer treatment regimens worldwide.
Cancer Types Treated with Adriamycin
Adriamycin is a highly effective chemotherapeutic agent used in treating a wide range of cancers. Its use is particularly prominent in:
- Acute Leukemia: Adriamycin is a crucial component of many treatment regimens for acute lymphocytic leukemia (ALL) and acute myeloid leukemia (AML), especially in adults. It’s often combined with other chemotherapy drugs in induction and consolidation phases to achieve remission and prevent relapse.
- Breast Cancer: Adriamycin is a standard treatment for aggressive breast cancers, particularly those that are HER2-positive. It’s frequently used in combination with other chemotherapy agents and targeted therapies like trastuzumab.
- Lung Cancer: Adriamycin is often included in treatment plans for small cell lung cancer (SCLC) and some non-small cell lung cancer (NSCLC) subtypes. It’s frequently used in combination with other chemotherapeutic agents and may be part of both initial and palliative treatment regimens.
- Hodgkin’s Lymphoma: Adriamycin is a cornerstone of treatment for Hodgkin’s lymphoma, often used in combination with other agents like bleomycin, vinblastine, and dacarbazine (ABVD regimen).
- Non-Hodgkin’s Lymphoma: Adriamycin is also used in treating various subtypes of non-Hodgkin’s lymphoma, often in combination with other chemotherapy drugs and targeted therapies.
- Ovarian Cancer: Adriamycin is a common component of treatment regimens for advanced ovarian cancer, often used in combination with other chemotherapy drugs like cisplatin.
- Sarcomas: Adriamycin is effective in treating various soft tissue and bone sarcomas, often used in combination with other chemotherapy drugs and radiation therapy.
- Multiple Myeloma: Adriamycin is sometimes used in combination with other drugs to treat multiple myeloma, particularly in patients with high-risk disease.
Regimens and Protocols for Adriamycin Administration
The specific regimen and protocol for Adriamycin administration vary depending on the type of cancer being treated, the patient’s overall health, and other factors. Some common regimens include:
- Single-Agent Therapy: In some cases, Adriamycin may be administered as a single agent, particularly in the treatment of certain types of leukemia or lymphoma.
- Combination Chemotherapy: More commonly, Adriamycin is used in combination with other chemotherapy drugs, often in cycles that alternate between different drug combinations. For example, the ABVD regimen for Hodgkin’s lymphoma involves alternating cycles of Adriamycin, bleomycin, vinblastine, and dacarbazine.
- Adjuvant Therapy: Adriamycin may be used as adjuvant therapy after surgery to reduce the risk of cancer recurrence.
- Neoadjuvant Therapy: Adriamycin can be used as neoadjuvant therapy before surgery to shrink the tumor and improve the chances of successful surgery.
Effectiveness of Adriamycin in Achieving Tumor Remission and Improving Patient Survival
Adriamycin has demonstrated significant effectiveness in achieving tumor remission and improving patient survival rates in various cancer types. Studies have shown that Adriamycin can:
- Induce Complete Remission: Adriamycin can induce complete remission in a significant proportion of patients with certain cancers, such as acute leukemia and Hodgkin’s lymphoma.
- Prolong Survival: Adriamycin has been shown to prolong survival in patients with various cancers, including breast cancer, lung cancer, and ovarian cancer.
- Improve Quality of Life: By effectively controlling cancer growth and symptoms, Adriamycin can improve the quality of life for patients with cancer.
Side Effects and Toxicity of Adriamycin
Adriamycin, a potent chemotherapeutic agent, is known for its effectiveness in treating various cancers. However, its use is often accompanied by significant side effects. These side effects, ranging from mild to life-threatening, are a crucial aspect of Adriamycin therapy and require careful management.
Cardiotoxicity
Adriamycin’s cardiotoxicity is a major concern, potentially leading to heart failure. This occurs due to Adriamycin’s ability to accumulate in heart muscle cells, causing damage to the mitochondria and impairing their function.
- Reduced Cardiac Output: Adriamycin’s effects on the heart can lead to a reduction in the heart’s ability to pump blood effectively, resulting in decreased cardiac output. This can manifest as shortness of breath, fatigue, and swelling in the legs and ankles.
- Arrhythmias: Adriamycin can disrupt the heart’s electrical activity, leading to irregular heart rhythms, such as tachycardia (fast heart rate) or bradycardia (slow heart rate).
- Heart Failure: In severe cases, Adriamycin-induced cardiotoxicity can progress to heart failure, requiring medical intervention.
Myelosuppression
Adriamycin is known for its myelosuppressive effects, meaning it can suppress the production of blood cells in the bone marrow. This can lead to a decrease in red blood cells (anemia), white blood cells (neutropenia), and platelets (thrombocytopenia).
- Anemia: Reduced red blood cell production can lead to fatigue, shortness of breath, and pale skin. This can be managed with blood transfusions or erythropoietin, a hormone that stimulates red blood cell production.
- Neutropenia: Low white blood cell counts increase the risk of infections. Patients with neutropenia require careful monitoring and may need antibiotics to prevent or treat infections.
- Thrombocytopenia: Reduced platelet count can lead to easy bruising and bleeding. Platelet transfusions may be necessary in severe cases.
Alopecia
Adriamycin can cause hair loss, a common side effect of chemotherapy. This occurs because Adriamycin can damage the hair follicles, interrupting the hair growth cycle.
- Temporary Hair Loss: In most cases, hair loss is temporary, and hair growth usually resumes after treatment is completed.
- Managing Alopecia: While there is no cure for Adriamycin-induced alopecia, patients can manage it by wearing wigs, hats, or scarves.
Adriamycin Resistance and Overcoming Resistance
Adriamycin, a potent chemotherapeutic agent, is widely used to treat various cancers. However, the effectiveness of Adriamycin can be hampered by the development of drug resistance in cancer cells. Adriamycin resistance poses a significant challenge to cancer treatment, often leading to treatment failure and poor patient outcomes.
Mechanisms of Adriamycin Resistance
Adriamycin resistance can arise through multiple mechanisms, each contributing to the cancer cell’s ability to evade the drug’s cytotoxic effects. These mechanisms can be broadly categorized as follows:
- Decreased Drug Accumulation: Cancer cells can develop mechanisms to reduce the intracellular concentration of Adriamycin. This can occur through:
- Reduced drug uptake: A decrease in the expression or activity of membrane transporters responsible for Adriamycin uptake can limit its entry into the cell.
- Increased drug efflux: Overexpression of drug efflux pumps, such as P-glycoprotein (P-gp), can actively pump Adriamycin out of the cell, preventing its accumulation to cytotoxic levels.
- Altered Drug Target: Adriamycin exerts its cytotoxic effects by intercalating into DNA and inhibiting topoisomerase II activity. Mutations in the DNA or topoisomerase II can alter their affinity for Adriamycin, reducing the drug’s effectiveness.
- Increased DNA Repair: Cancer cells may enhance their DNA repair mechanisms, allowing them to repair Adriamycin-induced DNA damage more efficiently, thus surviving the drug’s cytotoxic effects.
- Activation of Survival Pathways: Adriamycin can trigger various signaling pathways that promote cell survival, such as the Akt and NF-κB pathways. Activation of these pathways can counteract the apoptotic effects of Adriamycin, enabling cancer cells to survive and proliferate.
Impact of Adriamycin Resistance on Treatment Outcomes
The development of Adriamycin resistance significantly impacts treatment outcomes and patient prognosis.
- Treatment Failure: Adriamycin resistance can lead to treatment failure, as the drug becomes ineffective in controlling tumor growth.
- Disease Progression: The lack of effective treatment allows the cancer to progress, leading to a decline in patient health and survival.
- Limited Treatment Options: Resistance to Adriamycin can limit the available treatment options, making it challenging to find effective therapies for the patient.
Strategies for Overcoming Adriamycin Resistance
Several strategies are being investigated to overcome Adriamycin resistance and improve treatment outcomes:
- Combination Therapies: Combining Adriamycin with other chemotherapeutic agents that target different pathways or have different mechanisms of action can be effective. This approach aims to circumvent resistance mechanisms and enhance the overall cytotoxic effect.
- Example: Combining Adriamycin with cyclophosphamide, a DNA alkylating agent, can increase the effectiveness of Adriamycin by preventing the repair of Adriamycin-induced DNA damage.
- Targeted Therapies: Targeting specific resistance mechanisms can effectively overcome Adriamycin resistance. This can involve:
- Inhibiting drug efflux pumps: Drugs like verapamil and cyclosporine can inhibit the activity of P-gp, reducing drug efflux and increasing Adriamycin accumulation within the cell.
- Targeting DNA repair pathways: Inhibiting DNA repair mechanisms can enhance the effectiveness of Adriamycin by preventing the repair of Adriamycin-induced DNA damage.
- Blocking survival signaling pathways: Targeting specific kinases involved in survival pathways, such as Akt or NF-κB, can sensitize cancer cells to Adriamycin and enhance its apoptotic effects.
- Drug Delivery Strategies: Novel drug delivery strategies can improve Adriamycin accumulation in cancer cells and overcome resistance mechanisms.
- Liposomal encapsulation: Encapsulating Adriamycin in liposomes can improve its delivery to tumor cells and reduce its accumulation in normal tissues, potentially improving therapeutic efficacy and reducing side effects.
- Nanoparticle-based delivery: Nanocarriers can be engineered to target specific cancer cells and deliver Adriamycin directly to the tumor site, enhancing its efficacy and reducing systemic toxicity.
Adriamycin in Combination Therapy

Adriamycin, also known as Doxorubicin, is often used in combination with other chemotherapy drugs or targeted agents to enhance its effectiveness and broaden its therapeutic scope. This approach, known as combination therapy, leverages the synergistic effects of different drugs to target cancer cells more effectively, minimizing resistance and maximizing treatment outcomes.
Commonly Used Combination Therapies
Combining Adriamycin with other agents can create a powerful therapeutic arsenal. Some common examples include:
- Cyclophosphamide: This alkylating agent is often used in combination with Adriamycin for treating various cancers, including breast cancer, lymphoma, and leukemia. The combination of these two drugs is known as the “AC regimen” and is highly effective in treating these cancers.
- 5-Fluorouracil (5-FU): This antimetabolite drug, commonly used for treating colorectal cancer, can be combined with Adriamycin to enhance its effectiveness. This combination is particularly effective in treating metastatic colorectal cancer.
- Vincristine: This vinca alkaloid drug, which disrupts microtubule function, is often combined with Adriamycin and cyclophosphamide in the “CAV regimen” for treating acute lymphoblastic leukemia (ALL).
- Trastuzumab: This monoclonal antibody targets the HER2 protein, which is overexpressed in some breast cancers. Combining Adriamycin with Trastuzumab is effective in treating HER2-positive breast cancer.
- Rituximab: This monoclonal antibody targets CD20, a protein found on the surface of B cells. Combining Adriamycin with Rituximab is effective in treating certain types of lymphomas, such as diffuse large B-cell lymphoma (DLBCL).
Rationale for Combining Adriamycin
Combining Adriamycin with other agents is often beneficial due to several factors:
- Synergistic effects: Combining Adriamycin with other drugs can lead to synergistic effects, where the combined effect is greater than the sum of the individual effects. This can lead to increased efficacy and reduced doses of each drug, minimizing side effects.
- Multi-targeted approach: Different drugs target different aspects of cancer cell growth and survival. Combining Adriamycin with other agents that target different pathways can create a multi-targeted approach, making it more difficult for cancer cells to develop resistance.
- Preventing resistance: Cancer cells can develop resistance to individual drugs. Combining Adriamycin with other agents can help prevent the development of resistance by targeting multiple pathways simultaneously.
Benefits of Combination Therapy
Using Adriamycin in combination therapy offers several advantages:
- Increased efficacy: Combination therapy often leads to higher response rates and improved overall survival compared to single-agent therapy.
- Improved tumor control: Combining Adriamycin with other agents can help shrink tumors more effectively and prevent them from growing back.
- Reduced side effects: In some cases, combination therapy can allow for lower doses of each individual drug, leading to fewer side effects.
Challenges of Combination Therapy
While combination therapy offers numerous benefits, it also presents some challenges:
- Increased toxicity: Combining Adriamycin with other drugs can increase the risk of side effects, including heart toxicity, bone marrow suppression, and nausea.
- Drug interactions: Different drugs can interact with each other, potentially leading to unpredictable effects. Careful monitoring and dose adjustments are crucial.
- Complexity of treatment: Combination therapy requires careful planning and monitoring to ensure optimal efficacy and minimize toxicity.
Adriamycin and Personalized Medicine
Personalized medicine plays a crucial role in tailoring Adriamycin treatment to individual patient characteristics, aiming to maximize therapeutic efficacy while minimizing adverse effects. By leveraging genetic testing and other biomarkers, healthcare providers can predict patient response to Adriamycin therapy and optimize treatment strategies.
Genetic Testing and Biomarkers in Adriamycin Treatment
Genetic testing and biomarkers are valuable tools for predicting patient response to Adriamycin therapy. By identifying specific genetic variations or biomarkers associated with drug sensitivity or resistance, healthcare providers can tailor treatment plans based on individual patient profiles.
- Genetic testing can identify specific gene mutations that may influence Adriamycin efficacy or toxicity. For example, mutations in genes involved in drug metabolism or DNA repair pathways can affect how patients respond to Adriamycin.
- Biomarkers, such as tumor markers or protein expression levels, can provide insights into tumor characteristics and predict treatment response. For instance, elevated levels of certain tumor markers may indicate a higher likelihood of Adriamycin resistance.
Personalized Medicine Approaches to Optimize Adriamycin Treatment
Personalized medicine approaches can optimize Adriamycin treatment by:
- Tailoring drug dosage and scheduling based on individual patient characteristics. For example, patients with specific genetic variations may require lower doses or different treatment schedules to minimize side effects.
- Selecting appropriate combination therapies based on patient-specific factors. Genetic testing and biomarkers can help identify patients who may benefit from combining Adriamycin with other drugs that target specific pathways.
- Monitoring treatment response and adjusting therapy accordingly. Regular monitoring of tumor response and side effects allows for timely adjustments to Adriamycin treatment to maximize efficacy and minimize toxicity.
Future Directions for Adriamycin Research
Adriamycin, despite its long history and established efficacy, remains a subject of ongoing research. Scientists and clinicians are actively exploring ways to enhance its therapeutic potential, minimize its toxicity, and expand its applications in the fight against cancer.
Improving Adriamycin Delivery and Targeting
Effective drug delivery is crucial for maximizing therapeutic efficacy while minimizing side effects. Current research focuses on developing novel strategies to deliver Adriamycin specifically to tumor cells, thereby reducing damage to healthy tissues.
- Nanotechnology-based drug delivery systems: These systems encapsulate Adriamycin within nanoparticles, allowing for targeted delivery to tumor cells and improved drug accumulation within the tumor microenvironment. This approach has the potential to enhance the therapeutic index of Adriamycin by concentrating the drug at the target site while minimizing systemic exposure and toxicity.
- Antibody-drug conjugates (ADCs): These conjugates combine Adriamycin with antibodies that specifically bind to tumor cell surface receptors. This approach ensures targeted delivery of the drug to cancer cells while minimizing exposure to healthy tissues. The development of ADCs has revolutionized cancer therapy by improving drug efficacy and reducing side effects. For example, the ADC trastuzumab emtansine (Kadcyla), which targets HER2-positive breast cancer, has shown significant clinical benefits.
Overcoming Adriamycin Resistance
Adriamycin resistance remains a major challenge in cancer treatment. Research efforts are focused on developing strategies to overcome this resistance and restore the drug’s effectiveness.
- Combination therapy: Combining Adriamycin with other chemotherapeutic agents or targeted therapies can enhance its effectiveness and overcome resistance mechanisms. For instance, combining Adriamycin with the tyrosine kinase inhibitor imatinib has shown promise in treating chronic myeloid leukemia (CML).
- Modulating drug efflux pumps: Some cancer cells develop resistance by overexpressing drug efflux pumps, which actively transport Adriamycin out of the cell. Research is exploring inhibitors of these efflux pumps to enhance intracellular drug accumulation and restore sensitivity to Adriamycin.
- Targeting resistance pathways: Research is investigating the mechanisms underlying Adriamycin resistance and developing strategies to target these pathways. This includes exploring novel drugs that inhibit key proteins involved in resistance development, such as the DNA repair protein PARP-1.
Adriamycin in Personalized Medicine
Personalized medicine aims to tailor cancer treatment to the specific characteristics of each patient. Research is investigating the use of biomarkers to predict Adriamycin response and identify patients who are most likely to benefit from this drug.
- Genetic testing: Identifying genetic variations that influence Adriamycin metabolism and sensitivity can help predict drug response and guide treatment decisions. For example, mutations in the gene encoding the enzyme CYP3A4, which is involved in Adriamycin metabolism, can influence drug efficacy and toxicity.
- Tumor profiling: Analyzing tumor tissue for specific molecular markers can help identify patients who are most likely to respond to Adriamycin. This information can guide treatment decisions and optimize the use of Adriamycin in personalized medicine.
Adriamycin’s impact on cancer treatment has been profound, offering a lifeline to countless patients. Its effectiveness in achieving tumor remission and improving survival rates has cemented its position as a critical tool in the fight against cancer. However, the development of resistance and the potential for significant side effects continue to be areas of ongoing research and development. Scientists are tirelessly working to refine existing therapies and develop new Adriamycin analogues with improved efficacy and reduced toxicity, paving the way for even more personalized and effective cancer treatments in the future.
Adriamycin, a powerful chemotherapy drug, has been a mainstay in cancer treatment for decades. However, its use can be limited by its potential for severe side effects. Fortunately, newer therapies like calquence , a targeted therapy, are offering alternative options with potentially fewer adverse effects. Further research into the efficacy and safety of these new treatments, in comparison to traditional chemotherapy agents like adriamycin, is crucial to improving patient outcomes.