Cidofovir, a synthetic nucleoside analogue, has emerged as a potent antiviral agent with a remarkable ability to combat a range of viral infections. This antiviral drug works by inhibiting the replication of viruses, specifically targeting the DNA polymerase enzyme crucial for viral DNA synthesis. Cidofovir’s versatility extends to its various formulations, including intravenous, oral, and topical applications, enabling targeted treatment for diverse viral infections.
This comprehensive overview delves into the intricate workings of cidofovir, exploring its chemical structure, mechanism of action, therapeutic applications, pharmacokinetic properties, and potential adverse effects. We will also delve into the crucial aspects of resistance mechanisms, clinical trials, and future directions for this promising antiviral agent.
Cidofovir

Cidofovir is a synthetic nucleotide analogue antiviral medication used to treat various viral infections. Its unique chemical structure and mechanism of action make it an effective agent against DNA viruses, particularly cytomegalovirus (CMV). This comprehensive overview will delve into the intricacies of cidofovir, exploring its chemical properties, mechanism of action, and available formulations.
Chemical Structure and Molecular Properties
Cidofovir’s molecular structure resembles that of deoxycytidine monophosphate, a natural nucleotide found in DNA. Its chemical formula is C9H14N3O8P, and it has a molecular weight of 325.2 g/mol. The key feature of cidofovir is its phosphonoformate group, which replaces the hydroxyl group at the 5′ position of deoxycytidine. This unique modification plays a crucial role in cidofovir’s antiviral activity.
Cidofovir is a white, crystalline powder that is soluble in water and has a pKa of 2.7. Its high water solubility is essential for its systemic absorption and distribution throughout the body. The pKa value indicates that cidofovir is predominantly ionized at physiological pH, which contributes to its intracellular accumulation and interaction with viral enzymes.
Mechanism of Action
Cidofovir’s antiviral activity stems from its ability to inhibit viral DNA polymerase, a key enzyme responsible for replicating viral DNA. Cidofovir acts as a competitive inhibitor of viral DNA polymerase, competing with the natural deoxycytidine triphosphate (dCTP) substrate for binding to the enzyme’s active site.
Cidofovir’s phosphonoformate group binds to the active site of viral DNA polymerase, preventing the incorporation of dCTP into the growing DNA chain.
This inhibition of DNA synthesis effectively blocks viral replication and prevents the production of new viral particles.
Formulations
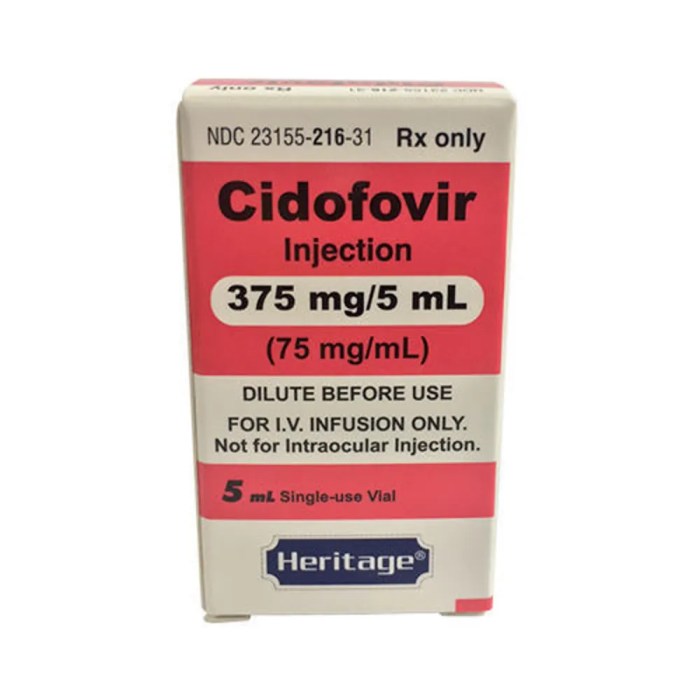
Cidofovir is available in two primary formulations for therapeutic use:
- Cidofovir Intravenous (IV) Formulation: This formulation is administered intravenously as a 10 mg/mL solution for treating CMV retinitis in patients with AIDS. It is typically given weekly for 2 weeks, followed by maintenance therapy every 2 weeks.
- Cidofovir Intravaginal Formulation: This formulation is available as a 1% cream for topical application to the vagina. It is used to treat human papillomavirus (HPV) infections, specifically genital warts.
Therapeutic Applications of Cidofovir
Cidofovir is a nucleotide analogue antiviral medication that has been approved for the treatment of several viral infections. It is a potent inhibitor of viral DNA polymerases, which are essential enzymes for viral replication. Cidofovir has been shown to be effective against a range of viruses, including cytomegalovirus (CMV), adenovirus, and papillomavirus.
Clinical Efficacy and Safety Profile, Cidofovir
Cidofovir has been shown to be effective in treating CMV retinitis in patients with AIDS. It is also used to treat other CMV infections, such as CMV pneumonitis and CMV esophagitis. In clinical trials, cidofovir has been shown to reduce the incidence of CMV retinitis and improve visual acuity in patients with AIDS. The safety profile of cidofovir is generally favorable, although it can cause some side effects, such as nephrotoxicity, neutropenia, and anemia.
Comparison with Other Antiviral Agents
Cidofovir is often used in combination with other antiviral agents, such as ganciclovir and valganciclovir, to treat CMV infections. The choice of antiviral agent depends on several factors, including the severity of the infection, the patient’s medical history, and the potential for drug interactions.
- For the treatment of CMV retinitis, cidofovir is often preferred over ganciclovir because it has a longer half-life and can be administered less frequently.
- However, cidofovir can cause more severe nephrotoxicity than ganciclovir, so it is important to monitor kidney function closely in patients receiving cidofovir.
- Valganciclovir is a prodrug of ganciclovir that is more bioavailable than ganciclovir. It is often used as an alternative to ganciclovir in the treatment of CMV retinitis.
- Cidofovir is also effective against adenovirus infections, but it is not the first-line treatment. Foscarnet is typically the first-line treatment for adenovirus infections, but cidofovir can be used if foscarnet is not effective or is poorly tolerated.
Pharmacokinetic and Pharmacodynamic Properties
Cidofovir’s pharmacokinetic profile is complex and influences its therapeutic efficacy. Its unique properties, including its slow absorption, limited distribution, and renal elimination, necessitate careful dosage and administration. Understanding these characteristics is crucial for optimizing its use in various clinical settings.
Absorption
Cidofovir’s absorption is slow and incomplete following oral administration. This is due to its poor bioavailability, which is less than 1%. Therefore, cidofovir is typically administered intravenously, allowing for direct entry into the systemic circulation and bypassing the first-pass metabolism in the liver.
Distribution
Cidofovir exhibits limited distribution in the body, with a low volume of distribution (Vd) of approximately 0.7 L/kg. This indicates that the drug primarily remains within the vascular compartment and has limited penetration into tissues. However, it can penetrate the cerebrospinal fluid (CSF) to a limited extent, reaching concentrations approximately 10-20% of those in plasma.
Metabolism
Cidofovir undergoes minimal metabolism in the body. It is primarily excreted unchanged in the urine, making renal function a key factor in its pharmacokinetic profile.
Excretion
Cidofovir is primarily eliminated through renal excretion. Its elimination half-life is approximately 2-3 hours in individuals with normal renal function. However, in patients with impaired renal function, the elimination half-life can be significantly prolonged, leading to drug accumulation and potential toxicity.
Factors Influencing Pharmacokinetic Profile
The pharmacokinetic profile of cidofovir can be influenced by several factors, including dosage, route of administration, and patient characteristics.
Dosage
The dosage of cidofovir is typically adjusted based on the patient’s renal function. In individuals with normal renal function, the recommended dose is 5 mg/kg administered intravenously once weekly. However, in patients with impaired renal function, the dosage may need to be reduced or the frequency of administration adjusted to prevent drug accumulation.
Route of Administration
As mentioned earlier, cidofovir is typically administered intravenously due to its poor oral bioavailability. However, alternative routes of administration, such as topical or intraocular, are being investigated for specific indications.
Patient Characteristics
Patient characteristics, such as age, weight, and renal function, can significantly influence the pharmacokinetic profile of cidofovir. For example, patients with impaired renal function may experience prolonged elimination half-lives, requiring dose adjustments.
Pharmacokinetic-Pharmacodynamic Relationship
The pharmacokinetic and pharmacodynamic properties of cidofovir are closely related. Its slow absorption and limited distribution contribute to its long half-life and the need for weekly dosing. The relationship between the drug’s concentration in the body and its antiviral activity is complex and influenced by the specific viral target. For example, cidofovir’s efficacy against cytomegalovirus (CMV) is directly correlated with its intracellular concentration.
The pharmacokinetic and pharmacodynamic properties of cidofovir are interconnected, influencing its therapeutic efficacy and potential for toxicity.
Adverse Effects and Drug Interactions
Cidofovir, while effective against various viral infections, can cause a range of adverse effects, some common and others rare. Understanding these effects and their management is crucial for safe and effective treatment. Additionally, potential interactions with other medications must be considered to minimize the risk of complications.
Common Adverse Effects
Common adverse effects of cidofovir treatment are generally mild to moderate in severity and often resolve with continued therapy or dose adjustment.
- Neutropenia: Cidofovir can suppress bone marrow function, leading to a decrease in neutrophil count, which are essential for fighting infections. This can increase the risk of infections, particularly those caused by bacteria and fungi.
- Renal dysfunction: Cidofovir can damage the kidneys, leading to elevated creatinine levels and decreased glomerular filtration rate. This risk is higher in patients with pre-existing renal impairment.
- Gastrointestinal disturbances: Nausea, vomiting, and diarrhea are common side effects of cidofovir, often occurring early in treatment. These symptoms can be managed with antiemetics and antidiarrheal medications.
- Elevated liver enzymes: Cidofovir can cause elevations in liver enzymes, indicating potential liver damage. Monitoring liver function is essential, especially in patients with pre-existing liver disease.
Rare Adverse Effects
While rare, cidofovir can cause serious adverse effects that require prompt medical attention.
- Pancreatitis: Inflammation of the pancreas can occur with cidofovir use, potentially leading to severe abdominal pain, nausea, and vomiting.
- Uveitis: Inflammation of the middle layer of the eye can occur, causing blurred vision, eye pain, and sensitivity to light.
- Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN): These rare but potentially life-threatening skin reactions can occur with cidofovir, characterized by widespread blistering and peeling of the skin.
Mechanisms Underlying Adverse Effects
The adverse effects of cidofovir are primarily attributed to its mechanism of action and its effects on various organ systems.
- Neutropenia: Cidofovir inhibits DNA polymerase, an enzyme crucial for cell replication. This inhibition can affect the bone marrow, leading to decreased production of neutrophils.
- Renal dysfunction: Cidofovir is primarily eliminated through the kidneys, and prolonged exposure can damage the renal tubules, leading to decreased filtration and electrolyte imbalances.
- Gastrointestinal disturbances: The exact mechanism is unclear, but it is believed that cidofovir can irritate the gastrointestinal tract, leading to nausea, vomiting, and diarrhea.
- Elevated liver enzymes: Cidofovir can accumulate in the liver, potentially causing damage to hepatocytes and leading to elevated liver enzymes.
Management of Adverse Effects
Managing adverse effects associated with cidofovir treatment involves a combination of strategies:
- Dose adjustment: Reducing the dose of cidofovir can often mitigate the severity of adverse effects, particularly neutropenia and renal dysfunction.
- Supportive care: Symptomatic treatment with antiemetics, antidiarrheal medications, and pain relievers can help manage gastrointestinal disturbances and pain.
- Monitoring: Regular monitoring of blood cell counts, renal function, and liver function is crucial to detect and manage potential complications.
- Discontinuation: In severe or persistent adverse effects, discontinuation of cidofovir treatment may be necessary.
Drug Interactions
Cidofovir can interact with other medications, potentially increasing the risk of adverse effects or decreasing the effectiveness of both drugs.
- Nephrotoxic drugs: Concomitant use of cidofovir with other nephrotoxic drugs, such as aminoglycosides, NSAIDs, and cyclosporine, can increase the risk of renal dysfunction.
- Drugs metabolized by the liver: Cidofovir can inhibit the cytochrome P450 enzyme system, potentially increasing the levels of other drugs metabolized by this system, leading to increased toxicity.
- Drugs affecting bone marrow: Cidofovir can enhance the myelosuppressive effects of other drugs that suppress bone marrow function, such as chemotherapy agents.
Recommendations for Safe Co-administration
To minimize the risk of drug interactions, it is crucial to:
- Thorough medical history: A comprehensive medical history should be obtained, including any pre-existing conditions, medications, and supplements.
- Careful monitoring: Close monitoring of renal function, liver function, and blood cell counts is essential during co-administration of cidofovir with other drugs.
- Dose adjustment: Dose adjustments of cidofovir or other interacting drugs may be necessary to minimize the risk of adverse effects.
- Alternative medications: If possible, alternative medications with fewer potential interactions should be considered.
Resistance Mechanisms and Management
Cidofovir resistance is a significant concern in the management of viral infections, particularly in patients with chronic infections or those receiving prolonged treatment. Understanding the mechanisms of resistance and developing strategies to manage it are crucial for optimizing therapeutic outcomes.
Mechanisms of Cidofovir Resistance
The development of cidofovir resistance is primarily attributed to mutations in the viral DNA polymerase gene. These mutations can alter the enzyme’s structure and function, leading to decreased binding affinity for cidofovir or reduced catalytic activity.
- Mutations in the active site: These mutations directly alter the amino acids involved in the binding of cidofovir to the DNA polymerase. This can lead to reduced affinity for the drug, hindering its ability to inhibit viral replication.
- Mutations outside the active site: Mutations in regions outside the active site can indirectly affect the enzyme’s function by altering its conformation or stability. These changes can also reduce the binding affinity for cidofovir or interfere with its catalytic activity.
Clinical Implications of Cidofovir Resistance
Cidofovir resistance can significantly impact the effectiveness of treatment and lead to treatment failure.
- Treatment failure: Resistant viral strains can continue to replicate despite cidofovir therapy, leading to persistent or worsening infections.
- Increased viral load: The emergence of resistant strains can result in a significant increase in viral load, potentially leading to complications and disease progression.
- Limited treatment options: The development of resistance to cidofovir can limit the available treatment options, as alternative antiviral agents may not be effective or have different side effects.
Management of Cidofovir Resistance
Managing cidofovir resistance requires a multi-faceted approach, including:
- Genetic testing: Identifying mutations associated with cidofovir resistance is crucial for guiding treatment decisions.
- Treatment optimization: Optimizing the dosage and frequency of cidofovir administration can help minimize the emergence of resistance.
- Combination therapy: Using cidofovir in combination with other antiviral agents can help delay the emergence of resistance and enhance therapeutic efficacy.
- Alternative antiviral agents: If resistance to cidofovir develops, alternative antiviral agents may be considered, depending on the specific viral infection and the patient’s clinical condition.
Role of Genetic Testing
Genetic testing plays a critical role in identifying and monitoring cidofovir resistance.
- Early detection: Genetic testing can identify mutations associated with resistance before clinical signs of resistance appear, allowing for timely adjustments in treatment strategies.
- Monitoring resistance: Regular genetic testing can monitor the emergence and spread of resistant strains, providing valuable information for guiding treatment decisions.
- Treatment guidance: Genetic testing results can help guide the selection of alternative antiviral agents or other treatment strategies for managing resistant infections.
Clinical Trials and Research
Cidofovir has been evaluated in numerous clinical trials for various indications, providing valuable insights into its efficacy and safety profile. Ongoing research is exploring novel cidofovir-based therapies and formulations, aiming to enhance its therapeutic potential. Future research directions focus on optimizing its use, addressing limitations, and expanding its therapeutic applications.
Key Findings from Clinical Trials
Clinical trials have demonstrated the efficacy of cidofovir in treating various viral infections, including cytomegalovirus (CMV) retinitis, adenoviral keratoconjunctivitis, and papillomavirus infections.
- In CMV retinitis, cidofovir has shown significant efficacy in reducing viral load and improving visual acuity. A meta-analysis of 11 randomized controlled trials involving 724 patients with CMV retinitis found that cidofovir was superior to ganciclovir in terms of visual acuity improvement and time to treatment failure.
- For adenoviral keratoconjunctivitis, cidofovir has been effective in treating severe cases, especially in immunocompromised patients. A study involving 20 patients with severe adenoviral keratoconjunctivitis found that cidofovir eye drops led to a significant reduction in corneal inflammation and visual impairment.
- In treating papillomavirus infections, cidofovir has shown promising results in reducing viral load and improving clinical symptoms. A study involving 27 patients with recurrent respiratory papillomatosis found that cidofovir treatment led to a significant reduction in the number and size of papillomas.
Cidofovir has also been studied for the treatment of other viral infections, including herpes simplex virus (HSV) and Epstein-Barr virus (EBV) infections. However, its efficacy in these indications is less established compared to CMV retinitis.
Ongoing Research on Novel Cidofovir-Based Therapies and Formulations
Research efforts are ongoing to develop novel cidofovir-based therapies and formulations to overcome limitations associated with current treatments.
- One focus is on developing more convenient and efficient drug delivery systems. For example, researchers are exploring the use of liposomal formulations of cidofovir to improve its bioavailability and reduce its nephrotoxicity.
- Another area of research involves developing novel cidofovir analogs with enhanced antiviral activity and reduced side effects. These analogs are designed to target specific viral enzymes or pathways, potentially leading to improved therapeutic outcomes.
These research efforts aim to optimize the therapeutic potential of cidofovir by enhancing its efficacy, reducing its toxicity, and expanding its therapeutic applications.
Future Research Directions to Optimize the Therapeutic Use of Cidofovir
Future research on cidofovir should focus on addressing its limitations and optimizing its therapeutic use.
- One important area of research is to further investigate the mechanisms of cidofovir resistance and develop strategies to overcome it. This could involve identifying novel drug targets or developing combination therapies that circumvent resistance mechanisms.
- Another research priority is to develop safer and more effective drug delivery systems. This could involve exploring alternative routes of administration, such as topical or inhaled formulations, to reduce systemic exposure and minimize side effects.
- Finally, further clinical trials are needed to evaluate the efficacy and safety of cidofovir in various indications, including emerging viral infections and rare diseases. This will provide valuable data to support its use in a wider range of clinical settings.
By addressing these research priorities, scientists can optimize the therapeutic use of cidofovir and expand its potential to treat a wider range of viral infections.
Patient Management and Monitoring
Cidofovir therapy requires careful management and monitoring due to its potential for serious adverse effects. Healthcare professionals play a crucial role in ensuring patient safety and efficacy throughout treatment.
Administration and Monitoring
The administration and monitoring of cidofovir therapy involve a comprehensive approach to minimize risks and optimize treatment outcomes.
Administration
- Cidofovir is typically administered intravenously over 1 hour.
- Dosage and frequency vary depending on the indication and patient factors.
- Prehydration with intravenous fluids is recommended to minimize nephrotoxicity.
- Close monitoring of renal function is essential, particularly during the initial phase of therapy.
Monitoring
- Regular monitoring of renal function is crucial, including serum creatinine, blood urea nitrogen (BUN), and estimated glomerular filtration rate (eGFR).
- Monitoring of liver function tests (LFTs) is also recommended to detect potential hepatotoxicity.
- Electrolyte levels, particularly potassium, should be monitored due to the risk of hypokalemia.
- Complete blood count (CBC) is recommended to assess for potential hematological abnormalities.
- Monitoring for signs and symptoms of adverse effects, such as nephrotoxicity, hepatotoxicity, and neutropenia, is essential.
Patient Education
Effective patient education is essential for ensuring adherence to treatment and managing potential adverse effects.
Common Concerns and Questions
- Potential side effects and how to manage them.
- Importance of regular monitoring and follow-up appointments.
- Lifestyle modifications, such as hydration and dietary changes, to minimize risks.
- Importance of adherence to medication schedule and reporting any unusual symptoms.
Role of Healthcare Professionals
Healthcare professionals play a critical role in managing and monitoring patients receiving cidofovir therapy.
Responsibilities
- Comprehensive assessment of patient history, including medical conditions, medications, and allergies.
- Informed consent and education regarding potential risks and benefits of cidofovir therapy.
- Close monitoring of renal function, LFTs, electrolytes, and CBC.
- Prompt management of adverse effects, including dose adjustments or discontinuation of therapy.
- Coordination with other healthcare providers involved in patient care.
Social and Ethical Considerations
Cidofovir’s therapeutic potential is undeniable, but its use raises significant social and ethical considerations. These issues are intertwined with accessibility, cost, potential misuse, and the unique challenges of treating specific patient populations.
Access to Treatment
Access to cidofovir therapy is crucial for individuals with life-threatening infections. However, several factors can hinder access, including:
- High Cost: Cidofovir’s cost can be a significant barrier, particularly in resource-limited settings. This can lead to disparities in treatment availability, with those in lower socioeconomic brackets facing greater difficulties.
- Limited Availability: Cidofovir may not be readily available in all healthcare facilities, especially in developing countries. This can be attributed to logistical challenges, limited infrastructure, and insufficient healthcare budgets.
- Lack of Insurance Coverage: The absence of comprehensive insurance coverage for cidofovir can make it financially inaccessible for many patients. This issue is particularly relevant in countries with limited or fragmented healthcare systems.
Cost Considerations
The high cost of cidofovir therapy raises concerns about its affordability and sustainability. This is particularly relevant in the context of long-term treatment for chronic infections.
- Financial Burden: The ongoing expense of cidofovir can impose a significant financial burden on individuals and families, potentially leading to treatment interruptions or abandonment.
- Healthcare System Strain: The high cost of cidofovir can strain healthcare budgets, diverting resources from other essential services. This can create a dilemma for policymakers who need to balance cost-effectiveness with patient access.
- Potential for Price Gouging: The limited availability and high demand for cidofovir can create opportunities for price gouging, further exacerbating affordability issues.
Potential Misuse
The misuse of cidofovir, like any powerful medication, poses a significant risk. This can occur in various ways:
- Self-Medication: Individuals may attempt to self-medicate with cidofovir without proper medical supervision, potentially leading to adverse effects or drug resistance.
- Unauthorized Distribution: Cidofovir may be illegally distributed or sold, bypassing regulatory oversight and quality control measures.
- Counterfeit Products: The availability of counterfeit cidofovir products can pose serious health risks, as these products may contain incorrect dosages, impurities, or inactive ingredients.
Ethical Considerations for Specific Patient Populations
The use of cidofovir in specific patient populations, such as pregnant women or children, raises unique ethical considerations.
Pregnant Women
The safety of cidofovir during pregnancy is a critical concern. While limited data suggest potential risks to the fetus, more research is needed to establish definitive guidelines.
- Limited Data: There is limited data on the safety of cidofovir during pregnancy, making it challenging to assess potential risks to the fetus.
- Potential Risks: Studies suggest potential risks to the fetus, including birth defects and developmental problems. However, the evidence is not conclusive.
- Balancing Risks and Benefits: Healthcare providers must carefully weigh the potential risks of cidofovir therapy against the benefits for pregnant women with life-threatening infections.
Children
The use of cidofovir in children also requires careful consideration, as their developing bodies may be more susceptible to adverse effects.
- Dosage Adjustments: Pediatric dosing of cidofovir is often adjusted based on age, weight, and renal function, requiring careful monitoring and individualized treatment plans.
- Potential for Toxicity: Children may be more susceptible to the toxic effects of cidofovir, necessitating close monitoring and potential adjustments to treatment regimens.
- Long-Term Effects: The long-term effects of cidofovir on children’s growth and development are not fully understood, requiring further research and careful evaluation.
Global Health Implications
Cidofovir’s use in the context of global health presents both challenges and opportunities.
- Addressing Health Disparities: Cidofovir’s use can help address health disparities by providing access to effective treatment for individuals in resource-limited settings.
- Combating Emerging Infections: Cidofovir’s potential to treat emerging infectious diseases, such as those caused by drug-resistant pathogens, is crucial for global health security.
- Sustainable Access: Ensuring sustainable access to cidofovir in developing countries requires addressing cost barriers, strengthening healthcare infrastructure, and promoting equitable distribution.
Future Directions and Emerging Trends
Cidofovir has proven its effectiveness in treating various viral infections, but ongoing research continues to explore new avenues to enhance its therapeutic potential. These efforts focus on developing novel formulations, optimizing drug delivery systems, and investigating combination therapies to overcome existing limitations and broaden its applicability. Furthermore, the integration of emerging technologies holds significant promise for advancing cidofovir’s development and clinical use.
Novel Formulations and Drug Delivery Systems
Novel formulations and drug delivery systems are being explored to improve the pharmacokinetic profile of cidofovir, enhance its bioavailability, and minimize adverse effects.
- Liposomal formulations: Encapsulating cidofovir within liposomes can improve its solubility, reduce its renal toxicity, and extend its half-life, leading to more sustained drug levels in the body. For instance, studies have shown that liposomal cidofovir exhibits increased efficacy against cytomegalovirus (CMV) infection in preclinical models, suggesting its potential for treating CMV retinitis in patients with compromised immune systems.
- Nanoparticle-based delivery systems: Nanoparticles can be engineered to target specific organs or tissues, delivering cidofovir directly to the site of infection, thereby maximizing its therapeutic efficacy and minimizing off-target effects. For example, nanoparticles coated with antibodies against CMV antigens have shown promising results in delivering cidofovir specifically to CMV-infected cells in vitro, suggesting their potential for targeted therapy in CMV retinitis.
- Oral formulations: Current cidofovir formulations require intravenous administration, which limits its convenience and patient compliance. Research is underway to develop oral formulations that would enhance patient adherence and improve the overall treatment experience. Oral formulations may also offer advantages in terms of cost-effectiveness and accessibility.
Cidofovir stands as a testament to the power of scientific innovation in combating viral infections. Its unique mechanism of action, diverse formulations, and ongoing research promise a brighter future for patients battling these challenging diseases. As we continue to unravel the intricacies of cidofovir, we can anticipate advancements in treatment strategies and a greater understanding of its role in global health.
Cidofovir is an antiviral medication used to treat certain viral infections, particularly cytomegalovirus (CMV) retinitis. It works by inhibiting the DNA polymerase of the virus, preventing its replication. While cidofovir is effective against CMV, it can have significant side effects. For the treatment of HIV, a combination of medications like emtricitabine tenofovir is often preferred. This combination targets different stages of the HIV lifecycle, leading to a more comprehensive and effective treatment approach.
Similar to cidofovir, these medications can also cause side effects, so careful monitoring and management are essential.