Oxymorphone, a potent synthetic opioid analgesic, stands as a powerful tool in managing severe pain, but its use is not without complexities. This drug, derived from morphine, acts on the central nervous system to alleviate pain, yet it also carries a risk of dependence and adverse effects. Understanding its intricacies, from its chemical structure to its therapeutic applications, is crucial for navigating the delicate balance between pain relief and potential complications.
Oxymorphone’s mechanism of action revolves around its binding to opioid receptors, primarily the mu receptor, triggering a cascade of events that ultimately result in pain suppression. However, this interaction also leads to a range of side effects, including respiratory depression, constipation, and sedation. Careful monitoring and dose adjustments are essential to manage these risks while maximizing therapeutic benefits.
Oxymorphone
Oxymorphone is a potent opioid analgesic that is used to treat moderate to severe pain. It is a synthetic opioid, meaning that it is not naturally occurring, but is made in a laboratory. Oxymorphone is a Schedule II controlled substance, meaning that it has a high potential for abuse and addiction.
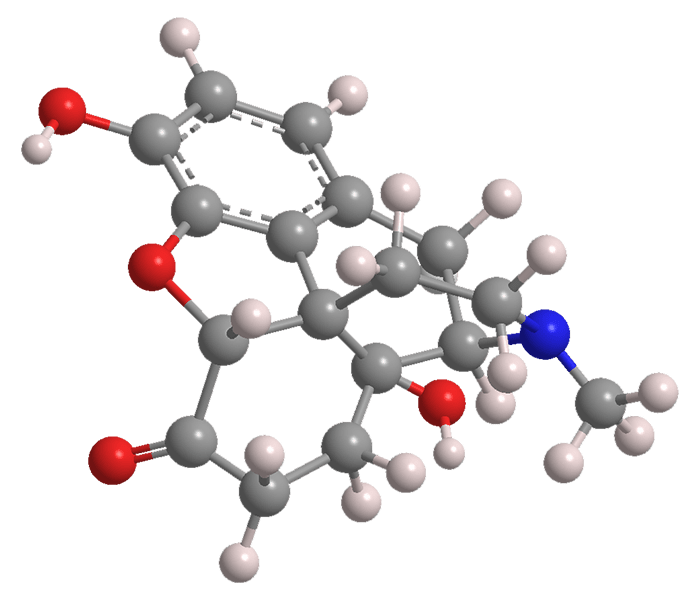
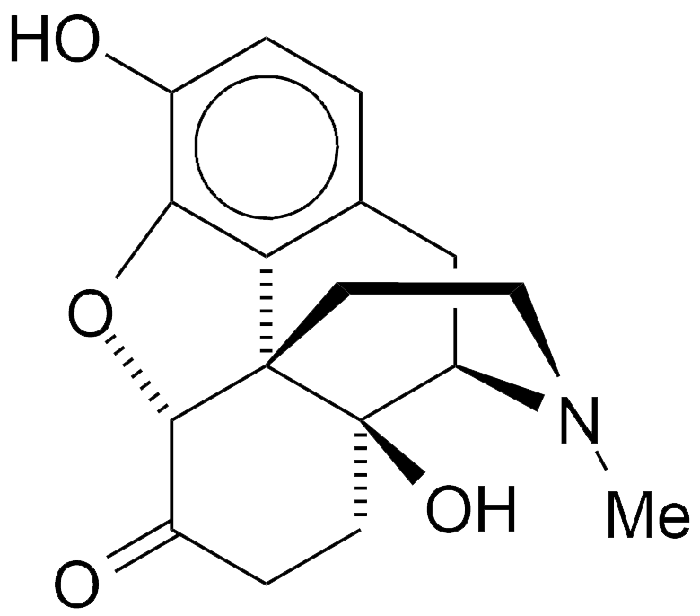
Chemical Structure and Properties
Oxymorphone is a semi-synthetic opioid analgesic derived from morphine. It is a white, crystalline powder that is practically odorless and has a bitter taste. The chemical formula for oxymorphone is C17H19NO4, and its molecular weight is 301.34 g/mol.
The chemical structure of oxymorphone is similar to that of morphine, but with a few key differences. The most significant difference is the presence of a ketone group at the C-14 position in oxymorphone, which is absent in morphine. This ketone group is responsible for the increased potency of oxymorphone compared to morphine.
Key Functional Groups
- Phenolic hydroxyl group: This group is present at the C-3 position and is responsible for the analgesic activity of oxymorphone. The phenolic hydroxyl group is involved in hydrogen bonding interactions with the opioid receptor, which is the primary target for oxymorphone.
- Tertiary amine group: This group is present at the C-17 position and is responsible for the basic properties of oxymorphone. The tertiary amine group can be protonated to form a positively charged ion, which is essential for the binding of oxymorphone to the opioid receptor.
- Ketone group: This group is present at the C-14 position and is responsible for the increased potency of oxymorphone compared to morphine. The ketone group is believed to increase the lipophilicity of oxymorphone, allowing it to cross the blood-brain barrier more easily and reach the opioid receptors in the brain.
Physical and Chemical Properties
- Solubility: Oxymorphone is soluble in water and alcohol, but insoluble in ether and chloroform.
- Stability: Oxymorphone is a relatively stable compound, but it can be degraded by light and heat.
- Melting Point: The melting point of oxymorphone is 156-158 °C.
Comparison with Morphine and Hydromorphone
Oxymorphone is a more potent opioid analgesic than morphine and hydromorphone. This is due to the presence of the ketone group at the C-14 position, which increases the lipophilicity of oxymorphone and allows it to cross the blood-brain barrier more easily.
The chemical structure of oxymorphone is very similar to that of morphine and hydromorphone, but the presence of the ketone group at the C-14 position makes oxymorphone a more potent analgesic.
The following table summarizes the chemical structures and pharmacological properties of morphine, hydromorphone, and oxymorphone:
| Opioid | Chemical Formula | Molecular Weight (g/mol) | Potency (relative to morphine) |
|---|---|---|---|
| Morphine | C17H19NO3 | 285.33 | 1 |
| Hydromorphone | C17H19NO3 | 285.33 | 5-7 |
| Oxymorphone | C17H19NO4 | 301.34 | 10-15 |
Oxymorphone
Oxymorphone is a potent opioid analgesic that acts on the central nervous system to relieve pain. Its mechanism of action involves binding to opioid receptors, primarily the mu (µ) receptor, leading to a cascade of events that ultimately result in pain reduction.
Opioid Receptor Interactions
Oxymorphone’s analgesic effects stem from its interaction with opioid receptors, specifically the mu (µ), kappa (κ), and delta (δ) subtypes. These receptors are G protein-coupled receptors (GPCRs) located in the central nervous system, particularly in the brain and spinal cord.
- Mu (µ) Receptor: Oxymorphone exhibits a high affinity for the µ receptor, which is the primary receptor responsible for its analgesic effects. Activation of the µ receptor leads to the inhibition of neurotransmitter release, primarily of excitatory neurotransmitters like glutamate and substance P, which are involved in pain signaling pathways. This inhibition of neurotransmitter release results in a reduction of pain perception.
- Kappa (κ) Receptor: While oxymorphone has a lower affinity for the κ receptor compared to the µ receptor, it can still activate this receptor. Activation of the κ receptor contributes to some of the side effects associated with oxymorphone, such as sedation, dysphoria, and respiratory depression.
- Delta (δ) Receptor: The δ receptor plays a lesser role in oxymorphone’s actions, although it may contribute to some of its analgesic effects.
Downstream Signaling Pathways
The binding of oxymorphone to opioid receptors initiates a series of downstream signaling events that lead to its pharmacological effects.
- G Protein Activation: Upon binding to opioid receptors, oxymorphone activates G proteins, which are intracellular signaling molecules.
- Adenylate Cyclase Inhibition: Activated G proteins inhibit the activity of adenylate cyclase, an enzyme that converts ATP into cyclic AMP (cAMP).
- cAMP Reduction: The inhibition of adenylate cyclase leads to a decrease in cAMP levels within the cell.
- Potassium Channel Activation: The reduction in cAMP levels activates potassium channels, leading to hyperpolarization of neurons and a decrease in neuronal excitability.
- Calcium Channel Inhibition: Oxymorphone also inhibits calcium channels, further reducing neuronal excitability and neurotransmitter release.
Oxymorphone
Oxymorphone is a potent opioid analgesic that is used to manage moderate to severe pain. Its pharmacokinetic profile plays a crucial role in determining its therapeutic efficacy and safety. This section delves into the pharmacokinetic properties of oxymorphone, exploring its absorption, distribution, metabolism, and elimination.
Pharmacokinetics of Oxymorphone
The pharmacokinetic profile of oxymorphone describes how the drug is absorbed, distributed, metabolized, and eliminated from the body. This understanding is essential for optimizing drug administration, managing potential side effects, and achieving desired therapeutic outcomes.
Absorption
Oxymorphone is available in various formulations, including oral tablets, extended-release tablets, and injectable solutions. The route of administration significantly influences its absorption.
- Oral Administration: When administered orally, oxymorphone undergoes significant first-pass metabolism in the liver, reducing its bioavailability. This means that only a fraction of the ingested dose reaches systemic circulation.
- Intravenous Administration: Intravenous (IV) administration bypasses the first-pass effect, leading to rapid and complete absorption. The drug quickly enters the bloodstream, resulting in a rapid onset of action.
- Intramuscular Administration: Intramuscular (IM) administration provides a slower absorption rate compared to IV administration. The drug is absorbed from the muscle tissue, reaching systemic circulation over a longer period.
Distribution
Once absorbed, oxymorphone distributes throughout the body, primarily binding to opioid receptors in the central nervous system (CNS) and other tissues. The drug’s distribution is influenced by factors such as blood flow, tissue permeability, and protein binding.
Oxymorphone has a high volume of distribution, indicating that it distributes extensively throughout the body tissues.
Metabolism
Oxymorphone is primarily metabolized in the liver by the enzyme CYP3A4. The major metabolite, oxymorphone-6-glucuronide, is inactive and excreted in the urine.
- Hepatic Function: Patients with impaired hepatic function may experience altered pharmacokinetic profiles, leading to increased drug accumulation and potential toxicity.
Elimination
Oxymorphone is eliminated from the body through a combination of metabolism and renal excretion.
- Renal Function: Patients with impaired renal function may exhibit prolonged elimination half-life, leading to drug accumulation and potential toxicity.
Factors Influencing Pharmacokinetics
Several factors can influence the pharmacokinetic properties of oxymorphone, including:
- Route of Administration: As mentioned earlier, the route of administration significantly affects absorption, leading to varying onset of action and bioavailability.
- Age: Elderly patients may exhibit reduced hepatic and renal function, leading to slower metabolism and elimination of oxymorphone.
- Hepatic Function: Liver disease can impair the metabolism of oxymorphone, leading to increased drug accumulation and potential toxicity.
- Renal Function: Kidney disease can affect the elimination of oxymorphone, leading to prolonged half-life and potential toxicity.
- Drug Interactions: Concomitant use of other medications, particularly those that inhibit CYP3A4, can alter the pharmacokinetic profile of oxymorphone.
Comparison with Other Opioid Analgesics
Oxymorphone’s pharmacokinetic profile is similar to other opioid analgesics, but there are some notable differences:
- Onset of Action: Oxymorphone has a relatively rapid onset of action, especially when administered intravenously. This makes it suitable for managing acute pain episodes.
- Duration of Action: The duration of action of oxymorphone varies depending on the formulation and route of administration. Extended-release formulations provide longer-lasting pain relief compared to immediate-release formulations.
- Bioavailability: Oral bioavailability of oxymorphone is lower compared to some other opioid analgesics, due to significant first-pass metabolism.
- Metabolism: Oxymorphone is primarily metabolized by CYP3A4, similar to many other opioids. However, the specific metabolites and their pharmacological activity can vary between different opioids.
Oxymorphone
Oxymorphone is a powerful opioid analgesic used to manage moderate to severe pain. It is a semi-synthetic opioid derived from thebaine, an alkaloid found in the opium poppy. Oxymorphone is available in various forms, including tablets, capsules, and injections, and is typically prescribed for short-term pain relief, but can be used long-term in certain situations.
Therapeutic Uses
Oxymorphone’s primary therapeutic indication is the management of moderate to severe pain. It is particularly effective for pain that is difficult to control with other analgesics, such as chronic pain, cancer pain, and neuropathic pain. Oxymorphone works by binding to opioid receptors in the central nervous system, which reduces the perception of pain.
Pain Conditions
Oxymorphone is commonly prescribed for various pain conditions, including:
- Acute pain: This refers to pain that is sudden and intense, often associated with injury or surgery. Oxymorphone can be used to manage acute pain in the short term, providing effective pain relief.
- Chronic pain: This refers to pain that persists for more than three months. Chronic pain can be caused by a variety of factors, including injury, disease, and medical conditions. Oxymorphone can be used to manage chronic pain in individuals who have not responded well to other analgesics.
- Cancer pain: Cancer pain is a common symptom of cancer, and it can be very severe. Oxymorphone is often used to manage cancer pain, especially when other pain medications are ineffective.
- Neuropathic pain: Neuropathic pain is caused by damage to the nerves. It can be a chronic and debilitating condition, often characterized by burning, tingling, or shooting pain. Oxymorphone can be effective in managing neuropathic pain, but it is important to note that it may not be effective for all types of neuropathic pain.
Benefits and Risks
The benefits of using oxymorphone for pain management include:
- Effective pain relief: Oxymorphone is a powerful analgesic that can provide significant pain relief for a wide range of pain conditions.
- Long-acting: Oxymorphone has a long duration of action, which can provide sustained pain relief.
- Multiple routes of administration: Oxymorphone is available in various forms, including tablets, capsules, and injections, allowing for flexibility in administration.
However, there are also risks associated with oxymorphone use, including:
- Addiction: Oxymorphone is an opioid, and like all opioids, it has the potential to cause addiction. This risk is increased with long-term use and high doses.
- Tolerance: Over time, the body can develop a tolerance to oxymorphone, requiring higher doses to achieve the same level of pain relief.
- Withdrawal: If oxymorphone is stopped abruptly after prolonged use, withdrawal symptoms can occur. These symptoms can be severe and include nausea, vomiting, diarrhea, muscle aches, and anxiety.
- Respiratory depression: Oxymorphone can slow down breathing, and in some cases, this can lead to respiratory depression. This is a serious risk, especially for individuals with pre-existing respiratory problems.
- Constipation: Constipation is a common side effect of opioid use, including oxymorphone.
- Drowsiness: Oxymorphone can cause drowsiness, which can impair driving or operating machinery.
Oxymorphone
Oxymorphone is a potent opioid analgesic used to manage moderate to severe pain. It is available in various formulations, including oral tablets, extended-release tablets, and injectable solutions. While effective in pain relief, oxymorphone, like other opioids, carries the risk of adverse effects, some of which can be serious.
Adverse Effects of Oxymorphone
Understanding the potential adverse effects of oxymorphone is crucial for safe and effective use. These effects can range from mild and manageable to severe and potentially life-threatening.
- Respiratory Depression: Oxymorphone’s primary mechanism of action involves binding to opioid receptors in the central nervous system, including the brainstem, where it inhibits the respiratory drive. This can lead to slowed breathing, shallow breaths, and, in severe cases, respiratory failure.
- Constipation: Oxymorphone can slow down gastrointestinal motility, leading to constipation. This effect is mediated by the opioid receptors in the gastrointestinal tract, which reduce peristalsis and increase intestinal transit time.
- Nausea and Vomiting: Nausea and vomiting are common adverse effects associated with oxymorphone. These effects are attributed to the stimulation of the chemoreceptor trigger zone (CTZ) in the brainstem, which is sensitive to opioids.
- Sedation: Oxymorphone can cause sedation due to its depressant effects on the central nervous system. This effect is primarily mediated by the opioid receptors in the brain, which can lead to drowsiness, lethargy, and impaired cognitive function.
- Dependence: Prolonged use of oxymorphone can lead to physical dependence. This means the body adapts to the presence of the drug, and withdrawal symptoms may occur upon abrupt cessation.
Managing Adverse Effects
Several strategies can be employed to manage or mitigate the adverse effects of oxymorphone:
- Dose Adjustment: Careful dose titration is essential to minimize adverse effects. Starting with a low dose and gradually increasing it as needed can help to optimize pain relief while minimizing side effects.
- Co-administration of Medications: Co-administration of medications can help to address specific adverse effects. For example, stool softeners or laxatives can help to prevent constipation, while antiemetics can reduce nausea and vomiting.
- Patient Education: Educating patients about the potential adverse effects of oxymorphone is crucial for safe and effective use. Patients should be advised to report any adverse effects to their healthcare provider promptly.
Oxymorphone
Oxymorphone is a potent opioid analgesic with a high potential for abuse and dependence. Its strong analgesic effects make it effective in managing severe pain, but its addictive properties require careful monitoring and management. This section delves into the potential for abuse and dependence associated with oxymorphone, exploring the underlying mechanisms and strategies for prevention and management.
Abuse and Dependence Potential
Oxymorphone’s potential for abuse and dependence stems from its pharmacological properties and the individual’s risk factors for opioid addiction. Its potent analgesic effects can lead to pleasurable feelings, reinforcing drug-seeking behavior. The risk of dependence is further amplified by the rapid development of tolerance, necessitating higher doses for the same effect, and the occurrence of withdrawal symptoms upon cessation.
Mechanisms of Opioid Dependence
Opioid dependence is characterized by a complex interplay of physiological and psychological factors. The primary mechanism involves neuroadaptation, where the brain adapts to the presence of opioids, leading to tolerance and withdrawal symptoms.
Tolerance
Tolerance develops as the body adapts to the repeated exposure to opioids, requiring higher doses to achieve the desired effect. This occurs due to the downregulation of opioid receptors and the desensitization of the central nervous system.
Withdrawal Symptoms
Withdrawal symptoms occur when the body is deprived of opioids after prolonged use. These symptoms can range from mild to severe and include:
- Muscle aches
- Nausea and vomiting
- Diarrhea
- Sweating
- Insomnia
- Restlessness
- Anxiety
- Irritability
The severity and duration of withdrawal symptoms depend on the duration and dosage of opioid use, as well as individual factors.
Strategies for Prevention and Management
Preventing and managing opioid dependence requires a multifaceted approach that addresses both the physiological and psychological aspects of addiction.
Harm Reduction Measures
Harm reduction strategies aim to minimize the negative consequences associated with opioid use. These measures include:
- Needle exchange programs
- Naloxone distribution
- Safe injection sites
Medication-Assisted Treatment
Medication-assisted treatment (MAT) involves the use of medications to manage withdrawal symptoms and reduce cravings. Commonly used medications include:
- Methadone
- Buprenorphine
- Naltrexone
MAT can be effective in reducing opioid use and improving overall health outcomes.
Behavioral Therapies
Behavioral therapies play a crucial role in addressing the psychological aspects of opioid dependence. These therapies aim to:
- Identify and manage triggers for drug use
- Develop coping mechanisms for cravings
- Improve social skills and support systems
- Address underlying mental health issues
Commonly used behavioral therapies include cognitive behavioral therapy (CBT), motivational interviewing, and contingency management.
Oxymorphone
Oxymorphone is a potent opioid analgesic that is available in various formulations for clinical use. These formulations differ in their bioavailability, duration of action, and ease of administration, making them suitable for different patient needs and clinical contexts.
Formulations and Administration
Oxymorphone is available in a variety of formulations, each with its own unique advantages and disadvantages. Understanding these differences is crucial for selecting the most appropriate formulation for individual patients.
- Oral Tablets: Oxymorphone oral tablets are available in immediate-release and extended-release formulations. Immediate-release tablets provide rapid pain relief, but their effects are relatively short-lived, requiring more frequent dosing. Extended-release tablets, on the other hand, provide sustained pain relief for a longer duration, typically 12 hours, reducing the need for frequent dosing.
- Injectable Solutions: Injectable solutions of oxymorphone are typically used for acute pain management, particularly in hospital settings. These formulations provide rapid and potent pain relief, making them suitable for situations requiring immediate pain control. However, they require skilled administration by healthcare professionals and may be associated with a higher risk of adverse effects.
- Transdermal Patches: Oxymorphone transdermal patches offer sustained pain relief for extended periods, typically 72 hours. They provide a consistent level of medication delivery through the skin, minimizing fluctuations in pain control. This formulation is particularly useful for chronic pain management and may be preferred for patients who find oral medications inconvenient or difficult to tolerate.
The choice of formulation and administration route depends on various factors, including the severity and type of pain, the patient’s individual needs and preferences, and potential drug interactions. Healthcare professionals play a crucial role in assessing these factors and determining the most appropriate formulation and dosage regimen for each patient.
Oxymorphone
Oxymorphone is a potent opioid analgesic used to manage moderate to severe pain. It is available in various formulations, including tablets, capsules, and extended-release injections. This section will delve into the crucial aspects of clinical monitoring and management of patients receiving oxymorphone therapy.
Clinical Monitoring and Management
It is essential to monitor patients receiving oxymorphone therapy closely to ensure optimal pain relief and minimize the risk of adverse effects.
- Vital Signs: Regular monitoring of vital signs, including blood pressure, heart rate, respiratory rate, and temperature, is crucial. Changes in these parameters can indicate potential complications like respiratory depression or cardiovascular instability.
- Pain Assessment: Regularly assess pain levels using a standardized pain scale, such as the Numeric Rating Scale (NRS) or the Visual Analog Scale (VAS). This helps determine the effectiveness of oxymorphone and guide dosage adjustments.
- Adverse Effect Surveillance: Monitor for common adverse effects associated with oxymorphone, such as constipation, nausea, vomiting, drowsiness, dizziness, and itching. Promptly address these issues to enhance patient comfort and safety.
- Drug Interactions: Be aware of potential drug interactions with oxymorphone, including other opioids, sedatives, and alcohol. Ensure that patients are fully informed about these interactions and the potential risks.
- Tolerance and Dependence: Monitor for signs of tolerance and dependence, which may require adjustments in dosage or consideration of alternative therapies.
Patient Management Protocol, Oxymorphone
A comprehensive protocol is essential for managing patients receiving oxymorphone therapy. This protocol should include:
- Initial Assessment: Conduct a thorough medical history and physical examination, including assessment of pain severity, underlying medical conditions, and potential drug interactions.
- Pain Level Assessment: Regularly assess pain levels using a standardized pain scale and document the findings. This helps determine the effectiveness of oxymorphone and guide dosage adjustments.
- Dosage Titration: Start with a low dose of oxymorphone and gradually increase it until adequate pain relief is achieved. The dosage should be individualized based on patient factors, including pain severity, weight, and tolerance. Monitor for signs of respiratory depression or other adverse effects during titration.
- Adverse Effect Management: Address adverse effects promptly and effectively. Constipation can be managed with stool softeners or laxatives. Nausea and vomiting may be treated with antiemetics. Drowsiness and dizziness may require dose adjustments or consideration of alternative medications.
- Drug Interaction Management: Educate patients about potential drug interactions with oxymorphone and advise them to avoid concurrent use of other opioids, sedatives, and alcohol.
- Tolerance and Dependence Management: Monitor for signs of tolerance and dependence. If tolerance develops, consider increasing the dosage or switching to a different opioid. Dependence can be managed through gradual dose reduction and appropriate supportive care.
- Patient Education: Provide patients with clear and concise information about oxymorphone, including its proper use, potential side effects, and the importance of adherence to the prescribed dosage and schedule. Educate them about the risks of misuse and dependence and encourage them to seek medical advice if they experience any concerns.
Patient Education and Communication
Effective patient education and communication are crucial in optimizing oxymorphone therapy and minimizing the risks of misuse or dependence.
- Informed Consent: Obtain informed consent from patients before initiating oxymorphone therapy. This ensures that patients understand the risks and benefits of the medication and are fully informed about the potential side effects and risks of misuse.
- Proper Use and Storage: Educate patients about the proper use of oxymorphone, including the correct dosage, timing, and administration route. Emphasize the importance of storing the medication securely and out of reach of children.
- Risk of Dependence: Discuss the risk of dependence with patients, particularly those with a history of substance abuse. Encourage them to seek help if they develop dependence and to avoid using the medication for non-medical purposes.
- Communication with Healthcare Provider: Encourage patients to communicate openly with their healthcare provider about any concerns or questions they may have regarding oxymorphone therapy. This includes reporting any adverse effects, changes in pain levels, or potential drug interactions.
Oxymorphone
Oxymorphone is a potent opioid analgesic that has been used for decades to manage moderate to severe pain. While it has proven effective, ongoing research and development efforts are continuously exploring new avenues to enhance its therapeutic profile and address its potential drawbacks. These efforts are focused on refining its formulations, exploring alternative routes of administration, and optimizing its safety and efficacy.
Future Directions in Oxymorphone Research
The development of novel formulations and alternative routes of administration aims to improve the convenience and efficacy of oxymorphone treatment.
- Extended-release formulations: These formulations aim to provide sustained pain relief over longer periods, reducing the frequency of dosing and improving patient adherence to treatment. Research is ongoing to develop extended-release oxymorphone formulations with improved pharmacokinetic profiles and reduced potential for abuse.
- Transdermal patches: Transdermal patches offer a non-invasive route of administration, potentially reducing the risk of injection-related complications and improving patient comfort. Research is investigating the feasibility and efficacy of transdermal oxymorphone patches for chronic pain management.
- Nasal sprays: Nasal sprays offer a rapid onset of action and may be suitable for managing breakthrough pain or acute pain episodes. Research is evaluating the safety and efficacy of oxymorphone nasal sprays.
Oxymorphone, while effective in treating severe pain, demands careful consideration due to its potential for dependence and adverse effects. Balancing its analgesic benefits with its risks requires a thorough understanding of its pharmacological properties, therapeutic applications, and potential interactions with other medications. Ongoing research continues to explore new formulations, alternative routes of administration, and strategies for improving its safety profile, paving the way for more effective and safer pain management.
Oxymorphone is a powerful opioid medication used to manage severe pain. While it’s often prescribed for chronic conditions, it’s important to note that there are other options available for managing everyday discomfort. For instance, services like hims pills offer telehealth consultations and prescription medications for a range of health concerns, including erectile dysfunction and hair loss. Returning to oxymorphone, it’s crucial to use it responsibly and under the guidance of a healthcare professional to minimize potential risks and ensure optimal treatment outcomes.