Levemir insulin sets the stage for this comprehensive exploration, offering readers a detailed understanding of its role in managing diabetes. Levemir, a long-acting insulin analog, provides a steady and extended release of insulin, helping to regulate blood sugar levels throughout the day.
This guide delves into the intricacies of Levemir insulin, covering its uses, administration, side effects, interactions, and more. We aim to equip individuals with valuable insights to make informed decisions regarding their diabetes management.
Levemir Insulin
Levemir insulin is a long-acting insulin analog used to control blood sugar levels in people with diabetes. It is a synthetic version of human insulin that has been modified to have a longer duration of action.
Mechanism of Action
Levemir insulin works by mimicking the natural insulin produced by the pancreas. Insulin helps glucose (sugar) enter cells, where it is used for energy. In people with diabetes, the pancreas either does not produce enough insulin or the body does not respond to insulin properly. Levemir insulin helps to lower blood sugar levels by providing a steady supply of insulin over a longer period.
Chemical Structure
Levemir insulin is a recombinant human insulin analog. It is produced by inserting the gene for human insulin into a bacterium, which then produces the insulin. Levemir insulin is chemically modified by adding a fatty acid chain to the insulin molecule. This modification slows down the absorption of the insulin into the bloodstream, resulting in a longer duration of action.
Uses and Indications

Levemir (insulin detemir) is a long-acting insulin analog used to control high blood sugar in adults and children with type 1 and type 2 diabetes. It is administered once or twice daily, providing a steady, long-lasting insulin effect for up to 24 hours.
How Levemir Insulin Works
Levemir insulin works by lowering blood sugar levels. It mimics the natural insulin produced by the pancreas, helping the body use glucose (sugar) for energy and reducing the amount of glucose in the bloodstream.
Conditions Treated
Levemir insulin is primarily used to treat the following conditions:
* Type 1 Diabetes: This condition occurs when the pancreas does not produce enough insulin. Levemir insulin helps replace the missing insulin, allowing the body to use glucose properly.
* Type 2 Diabetes: This condition develops when the body does not use insulin effectively, leading to high blood sugar levels. Levemir insulin helps improve insulin sensitivity and lower blood sugar levels.
Contraindications and Precautions
Levemir insulin is generally safe for most people, but there are some contraindications and precautions to consider:
Contraindications
* Hypoglycemia (low blood sugar): Individuals with hypoglycemia should not use Levemir insulin.
* Insulin allergy: People with a history of severe allergic reactions to insulin should not use Levemir.
Precautions
* Kidney or liver problems: Levemir insulin may need to be adjusted for people with kidney or liver problems.
* Pregnancy and breastfeeding: While Levemir insulin is safe for use during pregnancy and breastfeeding, it is important to discuss the risks and benefits with a healthcare professional.
* Driving and operating machinery: Hypoglycemia can cause dizziness, drowsiness, and impaired concentration, which may affect driving or operating machinery.
Administration and Dosage
Levemir insulin is typically administered once daily, at the same time each day, to help control blood sugar levels. The specific dosage and frequency will depend on your individual needs, as determined by your healthcare provider.
Dosage
Your doctor will determine the appropriate dosage of Levemir insulin based on your blood sugar levels, lifestyle, and other factors. The dosage may need to be adjusted over time to ensure optimal blood sugar control. It is important to follow your doctor’s instructions carefully and to monitor your blood sugar levels regularly.
Frequency of Administration
Levemir insulin is typically administered once daily, at the same time each day. The best time to administer Levemir insulin is usually in the evening, but your doctor may recommend a different time based on your individual needs.
Methods of Administration
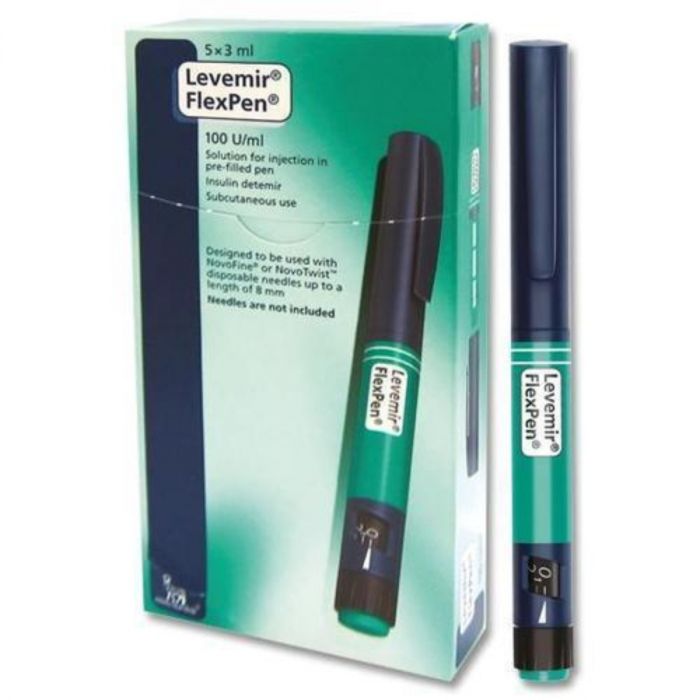
Levemir insulin is available in pre-filled pens and vials.
- Pre-filled pens are convenient and easy to use. They are designed to deliver a specific dose of insulin with each injection.
- Vials require the use of a separate syringe to draw up the insulin.
Storage and Handling
Proper storage and handling of Levemir insulin is essential to maintain its effectiveness.
- Refrigerate Levemir insulin vials and pre-filled pens before opening.
- Do not freeze Levemir insulin.
- Keep Levemir insulin out of direct sunlight and heat.
- Once opened, Levemir insulin can be stored at room temperature for up to 28 days.
- Dispose of used Levemir insulin pens and vials properly.
Side Effects and Risks
Like all medications, Levemir insulin can cause side effects. Most of these are mild and temporary, but some can be serious. It’s important to be aware of the potential side effects and to report any unusual symptoms to your doctor.
Common Side Effects
Common side effects of Levemir insulin are generally mild and often go away on their own. These include:
- Hypoglycemia (low blood sugar)
- Injection site reactions (redness, swelling, itching, or pain)
- Weight gain
- Fluid retention
Hypoglycemia is a common side effect of insulin therapy, and it can occur if you take too much insulin, miss a meal, or exercise more than usual. Symptoms of hypoglycemia can include:
- Shakiness
- Sweating
- Fast heartbeat
- Hunger
- Confusion
- Dizziness
- Headache
If you experience symptoms of hypoglycemia, you should immediately treat it by consuming a source of fast-acting carbohydrates, such as glucose tablets or juice. If your blood sugar doesn’t return to normal quickly, you may need to seek medical attention.
Potential Risks and Complications
While Levemir insulin is generally safe and effective, there are some potential risks and complications associated with its use. These include:
- Severe hypoglycemia: This is a serious condition that can lead to seizures, coma, and even death. It is more likely to occur if you take too much insulin, miss a meal, or exercise more than usual.
- Lipodystrophy: This is a condition that causes fat to build up or disappear at the injection site. It can be prevented by rotating injection sites.
- Allergic reactions: While rare, allergic reactions to Levemir insulin can occur. Symptoms of an allergic reaction can include:
- Hives
- Swelling
- Wheezing
- Difficulty breathing
If you experience an allergic reaction to Levemir insulin, you should stop using it and seek medical attention immediately.
- Diabetic retinopathy: This is a condition that affects the blood vessels in the retina of the eye. It can lead to vision loss. While Levemir insulin does not directly cause diabetic retinopathy, it is important to manage your blood sugar levels to help prevent this complication.
- Diabetic nephropathy: This is a condition that affects the blood vessels in the kidneys. It can lead to kidney failure. Like diabetic retinopathy, Levemir insulin does not directly cause diabetic nephropathy, but good blood sugar control is crucial to prevent it.
Interactions with Other Medications
Levemir insulin, like other medications, can interact with other drugs you may be taking. Understanding these interactions is crucial to ensure the safety and effectiveness of your treatment. These interactions can potentially affect how Levemir works in your body, leading to changes in blood sugar levels, increased risk of side effects, or reduced effectiveness of other medications.
Interactions with Other Medications
It’s important to inform your doctor about all the medications you are taking, including over-the-counter drugs, vitamins, and herbal supplements, before starting Levemir insulin. This includes prescription medications, such as:
- Oral medications for diabetes: Medications like sulfonylureas (e.g., glipizide, glyburide) and meglitinides (e.g., repaglinide, nateglinide) can increase the risk of low blood sugar (hypoglycemia) when combined with Levemir insulin. This is because these medications also stimulate insulin production and release, leading to an additive effect with Levemir.
- Beta-blockers: These medications, often used for high blood pressure or heart conditions, can mask the symptoms of low blood sugar, making it harder to recognize and treat. This can be dangerous as low blood sugar can lead to serious complications.
- Steroid medications: Steroids, such as prednisone, can raise blood sugar levels and reduce the effectiveness of Levemir insulin. This is because steroids have a counter-regulatory effect on insulin, making it harder for insulin to lower blood sugar.
- Certain antibiotics: Some antibiotics, like fluconazole and erythromycin, can increase the risk of low blood sugar when used with Levemir insulin. This is because these antibiotics can inhibit the breakdown of insulin in the body, leading to higher insulin levels.
Managing Medication Interactions
Your doctor will work with you to manage potential medication interactions. This may involve adjusting the dose of Levemir insulin or other medications, monitoring your blood sugar levels more frequently, or making lifestyle changes.
It is crucial to always talk to your doctor or pharmacist before taking any new medications while on Levemir insulin.
Monitoring and Management
Regular monitoring of blood glucose levels is essential for patients using Levemir insulin to ensure optimal blood sugar control and prevent complications. Healthcare professionals play a crucial role in guiding patients on effective monitoring and management strategies. Patient education and self-management skills are also vital for achieving successful outcomes.
Role of Blood Glucose Monitoring
Regular blood glucose monitoring is crucial for patients using Levemir insulin to achieve and maintain optimal blood sugar control. It helps in:
- Identifying trends in blood sugar levels: This allows for adjustments in insulin dosage or other aspects of the treatment plan as needed.
- Detecting hypoglycemia (low blood sugar): Early detection of hypoglycemia is essential for preventing serious complications.
- Monitoring the effectiveness of the insulin regimen: Regular monitoring helps ensure that the insulin is working effectively and that the dosage is appropriate.
- Identifying potential problems: Monitoring can help identify any underlying issues that may be affecting blood sugar control, such as infections or stress.
Role of Healthcare Professionals
Healthcare professionals play a vital role in monitoring and managing Levemir insulin therapy. They:
- Develop a personalized treatment plan: This includes determining the appropriate insulin dosage, injection schedule, and other management strategies.
- Monitor blood glucose levels: They will regularly check blood glucose levels during office visits and may recommend home monitoring.
- Adjust the treatment plan as needed: Based on blood glucose readings and other factors, healthcare professionals may adjust the insulin dosage, injection schedule, or other aspects of the treatment plan.
- Educate patients on self-management: They provide guidance on blood glucose monitoring, insulin administration, diet, exercise, and other aspects of managing diabetes.
- Address any concerns or questions: They provide support and guidance to patients throughout their treatment journey.
Patient Education and Self-Management
Patient education and self-management skills are essential for achieving optimal outcomes with Levemir insulin therapy. Patients should:
- Understand their diabetes: They should have a clear understanding of diabetes, its causes, and how it affects the body.
- Learn about Levemir insulin: They should understand the mechanism of action, dosage, injection technique, and potential side effects.
- Master blood glucose monitoring: They should learn how to use a blood glucose meter, interpret the readings, and record them accurately.
- Develop a healthy lifestyle: This includes maintaining a balanced diet, engaging in regular physical activity, and managing stress.
- Communicate with their healthcare team: They should openly discuss any concerns or questions with their healthcare professionals.
Comparison to Other Insulin Therapies

Levemir insulin is a long-acting insulin analog that is used to treat diabetes. It is one of several long-acting insulin therapies available, each with its own unique characteristics and benefits. Understanding the differences between these therapies is crucial for making informed decisions about treatment options.
The choice of insulin therapy depends on various factors, including the individual’s needs, lifestyle, and preferences. Each type of insulin has its own advantages and disadvantages, and it is important to discuss these with a healthcare professional to determine the best option for a specific patient.
Levemir insulin is a long-acting insulin that helps regulate blood sugar levels in individuals with diabetes. While Levemir is crucial for managing diabetes, it’s important to remember that managing mental health is equally important. If you’re experiencing anxiety, consider seeking help from a healthcare professional and exploring options like anti anxiety medication. Treating anxiety can positively impact your overall well-being and enhance your ability to effectively manage your diabetes with Levemir.
Comparison of Levemir Insulin to Other Long-Acting Insulin Therapies
Levemir insulin is compared to other long-acting insulin therapies, including:
- Detemir (Levemir): This is a long-acting insulin analog that provides a smooth and predictable insulin profile with a duration of action of up to 24 hours. It is typically administered once or twice daily, depending on individual needs.
- Glargine (Lantus, Toujeo): Glargine is another long-acting insulin analog with a duration of action of up to 24 hours. It is typically administered once daily and provides a more consistent insulin level throughout the day compared to Levemir.
- Degludec (Tresiba): Degludec is a very long-acting insulin analog with a duration of action of up to 42 hours. It is typically administered once daily and provides a more sustained insulin level, requiring less frequent injections compared to other long-acting insulins.
The table below summarizes the key differences between these long-acting insulin therapies:
| Insulin Therapy | Duration of Action | Administration Frequency | Key Features |
|---|---|---|---|
| Levemir (Detemir) | Up to 24 hours | Once or twice daily | Smooth and predictable insulin profile, typically administered once or twice daily. |
| Lantus, Toujeo (Glargine) | Up to 24 hours | Once daily | Provides a more consistent insulin level throughout the day, typically administered once daily. |
| Tresiba (Degludec) | Up to 42 hours | Once daily | Provides a more sustained insulin level, requiring less frequent injections compared to other long-acting insulins. |
Advantages and Disadvantages of Each Insulin Therapy
Each long-acting insulin therapy has its own advantages and disadvantages, which are summarized below:
Levemir (Detemir)
- Advantages:
- Provides a smooth and predictable insulin profile.
- Can be administered once or twice daily, offering flexibility in dosing schedules.
- Generally well-tolerated with a low risk of hypoglycemia.
- Disadvantages:
- May require more frequent adjustments to the dosage compared to other long-acting insulins.
- Can be associated with a higher risk of nocturnal hypoglycemia in some individuals.
Glargine (Lantus, Toujeo)
- Advantages:
- Provides a more consistent insulin level throughout the day.
- Typically administered once daily, reducing the frequency of injections.
- Generally well-tolerated with a low risk of hypoglycemia.
- Disadvantages:
- May require more frequent adjustments to the dosage compared to other long-acting insulins.
- Can be associated with a higher risk of nocturnal hypoglycemia in some individuals.
Degludec (Tresiba)
- Advantages:
- Provides a more sustained insulin level, requiring less frequent injections.
- May have a lower risk of nocturnal hypoglycemia compared to other long-acting insulins.
- Disadvantages:
- May have a higher risk of lipodystrophy (fat deposits) at the injection site.
- May be more expensive than other long-acting insulin therapies.
Specific Situations Where Levemir Insulin May Be Preferred
Levemir insulin may be preferred over other long-acting insulin therapies in specific situations, such as:
- Individuals with a preference for a smooth and predictable insulin profile: Levemir provides a more gradual onset of action and a smoother insulin profile compared to other long-acting insulins.
- Individuals with a flexible lifestyle: Levemir can be administered once or twice daily, offering flexibility in dosing schedules.
- Individuals with a history of nocturnal hypoglycemia: Levemir may have a lower risk of nocturnal hypoglycemia compared to other long-acting insulins, but it is important to note that individual responses can vary.
Research and Development
Levemir insulin, a long-acting insulin analog, has been a significant advancement in diabetes management since its introduction. However, ongoing research and development continue to explore ways to optimize its effectiveness, safety, and convenience for patients.
Ongoing Research and Development Efforts
Ongoing research and development efforts related to Levemir insulin focus on several key areas, aiming to improve its efficacy, safety, and patient experience. These efforts include:
- Developing more precise and predictable insulin delivery systems: Research is exploring new delivery methods, such as inhaled insulin or insulin patches, to provide more convenient and flexible insulin administration.
- Improving the duration of action: Researchers are investigating ways to extend the duration of action of Levemir insulin, potentially allowing for less frequent injections and better blood sugar control.
- Exploring new formulations: Studies are investigating different formulations of Levemir insulin, such as biosimilar versions, to ensure cost-effective and accessible treatment options.
- Investigating the role of Levemir insulin in specific populations: Research is examining the use of Levemir insulin in specific patient groups, such as children, pregnant women, and individuals with specific comorbidities, to understand its safety and efficacy in these populations.
Potential Future Applications and Advancements
The future of Levemir insulin therapy holds promising potential for advancements that could significantly impact diabetes management. These potential advancements include:
- Personalized insulin therapy: Future research may focus on developing personalized insulin regimens based on individual patient factors, such as genetics, lifestyle, and disease progression, to optimize blood sugar control.
- Combination therapies: Research is exploring the potential of combining Levemir insulin with other diabetes medications, such as GLP-1 receptor agonists, to achieve synergistic effects and improved glycemic control.
- Closed-loop systems: Advancements in artificial pancreas technology may integrate Levemir insulin with continuous glucose monitoring systems, allowing for automated insulin delivery and improved blood sugar management.
- Novel delivery systems: Ongoing research is exploring innovative delivery systems, such as implantable pumps or micro-needles, to provide continuous and precise insulin delivery, potentially eliminating the need for injections.
Ongoing Clinical Trials and Studies
Numerous clinical trials and studies are ongoing to evaluate the efficacy, safety, and long-term outcomes of Levemir insulin therapy. These studies aim to:
- Assess the effectiveness of Levemir insulin in different patient populations, including those with type 1 and type 2 diabetes, and those with specific comorbidities.
- Compare the efficacy and safety of Levemir insulin to other insulin therapies, including other long-acting insulins and newer insulin analogs.
- Evaluate the impact of Levemir insulin on long-term health outcomes, such as cardiovascular disease, kidney disease, and retinopathy.
- Explore the optimal dosing and administration strategies for Levemir insulin in different patient populations.
Patient Perspectives and Experiences
Living with diabetes requires a significant commitment to managing blood sugar levels, and insulin therapy plays a crucial role for many individuals. Levemir, a long-acting insulin, has helped countless people achieve better glycemic control and improve their quality of life. Understanding the perspectives and experiences of patients using Levemir is essential for providing comprehensive care and support.
Patient Experiences with Levemir
Patient experiences with Levemir can vary depending on individual factors, such as the severity of their diabetes, their lifestyle, and their adherence to the prescribed regimen. However, many patients report positive experiences with Levemir, citing its effectiveness in controlling blood sugar levels and its convenience due to its long-acting nature.
- Many patients appreciate the extended duration of action of Levemir, which typically lasts for 24 hours, reducing the frequency of insulin injections compared to shorter-acting insulins. This can lead to greater flexibility in meal planning and scheduling, making it easier to manage diabetes in daily life.
- Patients also often praise the predictable and consistent blood sugar control provided by Levemir, which can help reduce the risk of hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar).
- Some patients have reported that Levemir has helped them achieve better overall health and well-being, enabling them to engage in activities they previously found challenging due to their diabetes.
Impact of Levemir on Patients’ Lives, Levemir insulin
Levemir has a significant impact on the lives of patients with diabetes, influencing their daily routines, health outcomes, and overall quality of life.
- By providing effective blood sugar control, Levemir can help prevent or delay the onset of long-term diabetes complications, such as heart disease, stroke, nerve damage, and kidney disease. This can significantly improve patients’ long-term health and well-being.
- For many patients, Levemir has enabled them to lead more active and fulfilling lives, allowing them to participate in work, leisure activities, and social events without the constant worry about their blood sugar levels.
- Levemir can also have a positive impact on patients’ mental health and emotional well-being, as achieving better glycemic control can reduce feelings of stress, anxiety, and frustration associated with managing diabetes.
Benefits and Challenges of Levemir
Patients using Levemir generally acknowledge its benefits in controlling blood sugar levels and improving their overall health. However, they also recognize certain challenges associated with the therapy.
- One of the most common challenges reported by patients is the potential for injection site reactions, such as redness, swelling, or pain. These reactions are typically mild and temporary, but they can be uncomfortable for some individuals.
- Another challenge is the need for careful monitoring of blood sugar levels, as insulin therapy can lead to hypoglycemia if not managed properly. Patients must be vigilant about their blood sugar levels and adjust their insulin dosage accordingly.
- Some patients may also experience weight gain as a side effect of insulin therapy. This is due to the body’s increased utilization of glucose, leading to a higher calorie intake requirement. Patients can manage this by making lifestyle changes, such as adopting a healthy diet and increasing physical activity.
Patient Satisfaction with Levemir
Overall, many patients are satisfied with their experience using Levemir, reporting positive outcomes in terms of blood sugar control, quality of life, and overall health. However, it’s important to note that individual experiences can vary.
- Patients who have achieved good glycemic control with Levemir and have minimal side effects are generally very satisfied with the therapy. They appreciate the convenience and effectiveness of Levemir in managing their diabetes.
- Patients who experience more frequent or severe side effects or who find it difficult to manage their blood sugar levels effectively with Levemir may be less satisfied with the therapy. They may need to explore alternative insulin therapies or adjust their treatment regimen.
Cost and Accessibility: Levemir Insulin
The cost of Levemir insulin can be a significant financial burden for patients, especially those without adequate health insurance coverage. The high cost of insulin, including Levemir, has been a major concern for patients and healthcare providers alike.
Factors Influencing the Cost of Levemir Insulin
Several factors contribute to the high cost of Levemir insulin. These include:
- Research and Development Costs: Developing new medications, including insulin therapies, requires extensive research, clinical trials, and regulatory approvals. These costs are often passed on to consumers in the form of higher prices.
- Manufacturing Costs: The production of insulin involves complex processes and specialized equipment, which can contribute to the overall cost of the medication.
- Market Dynamics: The insulin market is dominated by a few major pharmaceutical companies, which can influence pricing strategies and limit competition.
- Insurance Coverage: The extent of insurance coverage for insulin can vary significantly, impacting the out-of-pocket costs for patients. Some insurance plans may have high co-pays or deductibles for insulin, making it difficult for patients to afford their medication.
- Lack of Generic Options: While generic versions of some insulin medications are available, there are no generic options for Levemir. This lack of competition can contribute to higher prices.
Initiatives and Programs Aimed at Improving Access to Levemir Insulin
Various initiatives and programs are being implemented to address the affordability and accessibility of insulin for patients. These include:
- Patient Assistance Programs: Many pharmaceutical companies, including Novo Nordisk, which manufactures Levemir, offer patient assistance programs (PAPs) to help eligible patients afford their medications. These programs provide financial assistance or discounts on insulin based on income and other criteria.
- State-Level Programs: Some states have implemented programs to provide financial assistance or access to insulin for low-income individuals. These programs may offer subsidies, co-pay assistance, or access to discounted insulin through state-run pharmacies.
- Affordable Care Act: The Affordable Care Act (ACA) has expanded health insurance coverage to millions of Americans, including those with pre-existing conditions such as diabetes. This expansion has improved access to healthcare services, including insulin therapies, for many individuals.
- Price Negotiation: Some organizations are advocating for increased price negotiation for insulin, arguing that the current pricing structure is unsustainable. This could involve government negotiations with pharmaceutical companies to lower insulin prices or the introduction of price caps on insulin.
Understanding Levemir insulin is crucial for individuals living with diabetes. From its mechanism of action to its potential side effects and interactions, this guide has provided a comprehensive overview. Remember, regular blood glucose monitoring, adherence to prescribed dosages, and close communication with healthcare professionals are essential for safe and effective management of diabetes using Levemir insulin.