Buprenorphine naloxone, a medication often prescribed for opioid use disorder, presents a unique approach to treatment. This combination drug, known for its effectiveness in managing cravings and reducing withdrawal symptoms, offers hope for individuals seeking recovery from opioid addiction. The inclusion of naloxone, a potent opioid antagonist, serves as a safety net, mitigating the risk of overdose by blocking the effects of opioids. This article delves into the intricacies of buprenorphine naloxone, exploring its mechanism of action, medical uses, safety considerations, and the evolving landscape of research and development.
Understanding the nuances of buprenorphine naloxone is crucial for healthcare professionals, patients, and their families. This comprehensive guide provides a detailed overview of the medication, its potential benefits and risks, and the essential aspects of its management. From its pharmacokinetic properties to the legal and regulatory aspects surrounding its use, this resource aims to empower individuals with the knowledge necessary to navigate this complex topic.
Buprenorphine Naloxone

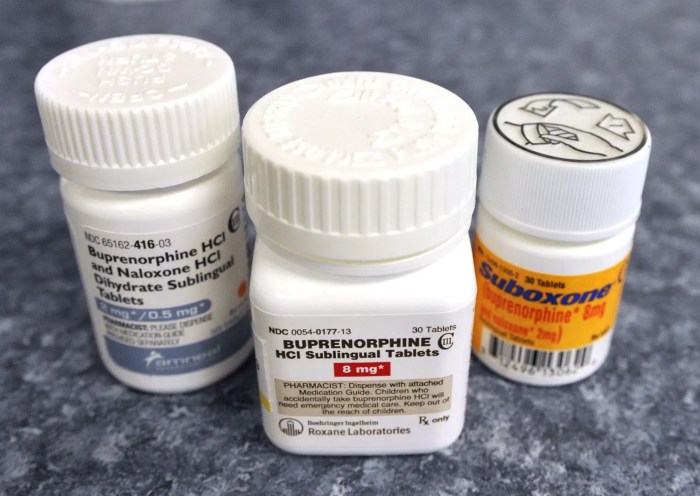
Buprenorphine naloxone is a medication used for the treatment of opioid use disorder. It is a combination of two medications: buprenorphine, a partial opioid agonist, and naloxone, an opioid antagonist. This medication is available in various formulations, including sublingual films, tablets, and injections, and is commonly prescribed to individuals struggling with opioid addiction.
Mechanism of Action
Buprenorphine and naloxone work together to reduce opioid cravings and withdrawal symptoms while preventing opioid overdose. Buprenorphine binds to opioid receptors in the brain, producing a partial agonist effect, meaning it activates the receptors but to a lesser degree than full opioid agonists like heroin or morphine. This results in a reduction of cravings and withdrawal symptoms without the intense euphoric effects associated with full agonists.
Naloxone, on the other hand, acts as an opioid antagonist, blocking the effects of other opioids. Its presence in buprenorphine naloxone formulations serves as a safety measure, mitigating the risk of overdose. If someone were to take a large dose of heroin or other opioids while on buprenorphine naloxone, the naloxone would counteract the effects of the opioid, preventing a potentially fatal overdose.
Role of Naloxone in Mitigating Opioid Overdose Risk
Naloxone plays a crucial role in mitigating the risk of opioid overdose by blocking the effects of opioids at the opioid receptors. When an individual takes an opioid, it binds to these receptors, leading to a range of effects, including respiratory depression, which can be fatal. Naloxone, by competitively binding to the same receptors, displaces the opioid and reverses its effects.
Formulations of Buprenorphine Naloxone
Buprenorphine naloxone is available in various formulations, each with its own unique characteristics and advantages:
- Sublingual Film: This formulation is a thin, dissolvable film placed under the tongue, offering a convenient and discreet method of administration. It is absorbed quickly and is often preferred for its ease of use.
- Tablet: Buprenorphine naloxone tablets are taken orally and are typically swallowed with water. They offer a more traditional method of administration, but may take longer to be absorbed than sublingual films.
- Injection: Injectable buprenorphine naloxone is administered by a healthcare professional and is typically used in emergency settings or for individuals who cannot tolerate oral formulations. It provides a rapid onset of action and can be particularly helpful in reversing opioid overdose.
Medical Uses and Indications
Buprenorphine naloxone is a medication primarily prescribed for the treatment of opioid use disorder (OUD). Its unique combination of a partial opioid agonist (buprenorphine) and an opioid antagonist (naloxone) makes it a valuable tool for managing opioid withdrawal symptoms and preventing relapse.
Treatment of Opioid Use Disorder, Buprenorphine naloxone
Buprenorphine naloxone is highly effective in treating opioid use disorder. It works by attaching to opioid receptors in the brain, partially activating them to reduce cravings and withdrawal symptoms. Naloxone blocks the effects of heroin and other opioids, preventing a high and discouraging relapse.
- Reduces withdrawal symptoms: Buprenorphine reduces the intensity and duration of withdrawal symptoms like muscle aches, sweating, nausea, and anxiety. This makes it easier for individuals to manage their withdrawal and stay engaged in treatment.
- Decreases cravings: Buprenorphine’s partial agonist activity helps reduce cravings for opioids, making it easier for individuals to resist relapse.
- Prevents overdose: Naloxone in the formulation acts as a safety net, blocking the effects of opioids in case of accidental overdose.
- Improves quality of life: Treatment with buprenorphine naloxone can lead to significant improvements in overall well-being, allowing individuals to regain control of their lives and participate more fully in their communities.
Pain Management
While buprenorphine naloxone is primarily used for opioid use disorder, it can also be prescribed for pain management in certain situations. It is generally considered a second-line option for chronic pain, typically after other pain medications have been tried.
- Chronic pain: Buprenorphine can be effective for managing chronic pain, especially in individuals with a history of opioid use disorder or those at high risk for addiction.
- Post-surgical pain: Buprenorphine can be used for pain management after surgery, especially for patients with a history of opioid use disorder.
Pharmacokinetics and Drug Interactions
Buprenorphine naloxone is a medication that is absorbed, distributed, metabolized, and excreted by the body. Understanding these pharmacokinetic processes is crucial for determining the appropriate dosage and frequency of administration, as well as for predicting potential drug interactions.
Absorption
Buprenorphine naloxone is typically administered sublingually, meaning it is placed under the tongue. This route of administration allows for rapid absorption into the bloodstream, bypassing the first-pass metabolism in the liver. The bioavailability of buprenorphine naloxone, which is the fraction of the drug that reaches systemic circulation, is approximately 60%.
Distribution
Once absorbed, buprenorphine naloxone distributes throughout the body, binding to opioid receptors in the central nervous system (CNS) and other tissues. The drug has a high affinity for these receptors, resulting in a long duration of action. The volume of distribution of buprenorphine naloxone is approximately 1.5 liters per kilogram, indicating that it distributes widely throughout the body.
Metabolism
Buprenorphine naloxone is metabolized primarily in the liver by cytochrome P450 enzymes, particularly CYP3A4. The metabolism of buprenorphine produces several metabolites, some of which may also have opioid activity. Naloxone, the antagonist component of the medication, is also metabolized in the liver, but its metabolites are inactive.
Excretion
The metabolites of buprenorphine naloxone are excreted primarily in the urine, with a small amount excreted in the feces. The elimination half-life of buprenorphine, which is the time it takes for the drug concentration in the body to decrease by half, is approximately 36 hours. This long half-life contributes to the sustained effects of buprenorphine naloxone.
Drug Interactions
Buprenorphine naloxone can interact with other medications, potentially affecting their efficacy or safety. These interactions can occur due to several mechanisms, including:
- Competition for the same metabolic pathways
- Altered drug absorption
- Modification of drug elimination
- Synergistic or antagonistic effects at the receptor level
Potential Drug Interactions
- CYP3A4 Inhibitors: Medications that inhibit CYP3A4, such as ketoconazole, ritonavir, and grapefruit juice, can increase the levels of buprenorphine in the body, potentially leading to increased side effects. This is because CYP3A4 is the primary enzyme responsible for metabolizing buprenorphine.
- CYP3A4 Inducers: Medications that induce CYP3A4, such as rifampin, carbamazepine, and St. John’s wort, can decrease the levels of buprenorphine in the body, potentially reducing its effectiveness. These medications accelerate the metabolism of buprenorphine, leading to lower plasma concentrations.
- Opioid Agonists: Concomitant use of buprenorphine naloxone with other opioid agonists, such as morphine, codeine, or heroin, can increase the risk of respiratory depression and other adverse effects. This is due to the additive effects of these medications on the central nervous system.
- CNS Depressants: Medications that depress the central nervous system, such as benzodiazepines, barbiturates, and alcohol, can enhance the sedative effects of buprenorphine naloxone, increasing the risk of respiratory depression and coma.
- Antacids: Antacids can decrease the absorption of buprenorphine naloxone, potentially reducing its effectiveness. This is because antacids can alter the pH of the stomach, affecting the solubility and absorption of the medication.
Implications for Patient Management
It is crucial for healthcare professionals to be aware of potential drug interactions with buprenorphine naloxone. A thorough medication history is essential, including over-the-counter medications, herbal supplements, and illicit drug use. Patients should be advised to inform their healthcare provider of any changes in their medication regimen. Close monitoring for adverse effects, including respiratory depression, sedation, and withdrawal symptoms, is recommended, especially during the initiation of buprenorphine naloxone therapy and when there are changes in the patient’s medication regimen.
Safety and Side Effects
Buprenorphine naloxone, like any medication, can cause side effects. Understanding these potential effects is crucial for both patients and healthcare providers. It’s important to remember that not everyone experiences side effects, and their severity can vary greatly.
Common Side Effects
Common side effects of buprenorphine naloxone are generally mild and often subside as the body adjusts to the medication.
- Constipation: This is one of the most frequent side effects, often experienced by individuals taking buprenorphine naloxone. Staying hydrated, increasing fiber intake, and regular exercise can help manage this.
- Nausea and Vomiting: These side effects can occur, particularly during the initial days of treatment. Eating smaller, more frequent meals and avoiding fatty foods can help minimize discomfort.
- Drowsiness: Buprenorphine can cause drowsiness, especially during the initial phase of treatment. It’s important to avoid driving or operating machinery until you understand how the medication affects you.
- Headache: Headaches are a common side effect, often mild and temporary. Over-the-counter pain relievers can help manage headache symptoms.
- Sweating: Increased sweating is another common side effect, which may be more pronounced during the initial stages of treatment.
- Muscle aches: Muscle aches can occur, particularly during the initial days of treatment.
Serious Side Effects
While less common, serious side effects can occur. It’s important to seek immediate medical attention if you experience any of the following:
- Respiratory Depression: Buprenorphine can slow down breathing, particularly at higher doses. This is more likely to occur if you are taking other medications that depress the central nervous system, such as benzodiazepines.
- Overdose: Overdose can occur if you take more than the prescribed dose or if you mix buprenorphine naloxone with other substances, such as alcohol or benzodiazepines. Symptoms of overdose include slow breathing, drowsiness, confusion, and loss of consciousness.
- Allergic Reactions: Allergic reactions to buprenorphine naloxone are rare but can be serious. Symptoms of an allergic reaction include rash, itching, swelling, and difficulty breathing.
- Withdrawal Syndrome: Abruptly stopping buprenorphine naloxone can trigger withdrawal symptoms, which can be uncomfortable and potentially dangerous.
Withdrawal Syndrome
Withdrawal syndrome is a common concern for individuals taking buprenorphine naloxone. This is because buprenorphine is a partial opioid agonist, meaning it can trigger withdrawal symptoms if stopped abruptly. It is crucial to work with a healthcare provider to taper off buprenorphine naloxone gradually to minimize the risk of withdrawal symptoms.
Managing Withdrawal Symptoms
If withdrawal symptoms do occur, they typically manifest as:
- Flu-like symptoms: Runny nose, muscle aches, and chills.
- Restlessness: Difficulty sitting still or staying focused.
- Insomnia: Difficulty falling asleep or staying asleep.
- Yawning: Excessive yawning.
- Diarrhea: Loose stools or frequent bowel movements.
- Nausea and Vomiting: Feeling sick to your stomach or throwing up.
- Increased heart rate: A faster than normal heartbeat.
- Increased blood pressure: Higher than normal blood pressure.
- Sweating: Excessive sweating.
- Cravings: Intense desire to use opioids.
It’s important to note that withdrawal symptoms can be uncomfortable but are generally not life-threatening. Working closely with a healthcare provider to manage these symptoms is essential. They may recommend medications or other therapies to help ease the discomfort and manage cravings.
Monitoring for Adverse Events
Regular monitoring for adverse events is crucial when taking buprenorphine naloxone. Healthcare providers will typically assess your overall health, monitor for any side effects, and adjust your dosage as needed. Open and honest communication with your healthcare provider is essential to ensure the safe and effective use of buprenorphine naloxone.
Dosage and Administration
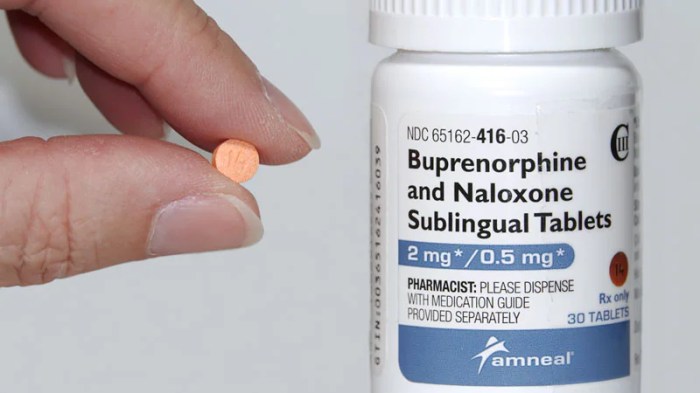
Buprenorphine naloxone is available as a sublingual film or tablet, and the dosage and administration will vary based on the individual patient’s needs. It’s crucial to tailor the treatment plan to the patient’s unique characteristics and medical history.
Dosage and Frequency
The recommended starting dose of buprenorphine naloxone is 8 mg/2 mg once daily. This dose can be adjusted based on the patient’s response and tolerance. The maximum daily dose is 32 mg/8 mg.
Administration
Buprenorphine naloxone should be administered sublingually, meaning it is placed under the tongue and allowed to dissolve. It is important to avoid chewing or swallowing the film or tablet. Patients should be instructed to allow the medication to dissolve completely, which typically takes 5-10 minutes.
Patient Education and Counseling
Patient education and counseling are critical components of successful buprenorphine naloxone treatment. Patients should be informed about the following:
- The importance of taking the medication as prescribed.
- The potential side effects of buprenorphine naloxone.
- The importance of regular follow-up appointments with their healthcare provider.
- The risks of using buprenorphine naloxone with other medications or substances.
- The importance of avoiding alcohol while taking buprenorphine naloxone.
- The signs and symptoms of an overdose and what to do in case of an overdose.
Treatment Considerations and Management
Managing patients on buprenorphine naloxone requires a multifaceted approach that considers various factors influencing treatment outcomes. This section explores key considerations for effective management, emphasizing the importance of addressing co-occurring mental health conditions and promoting long-term recovery from opioid addiction.
Key Considerations for Managing Patients on Buprenorphine Naloxone
The following table Artikels key considerations for managing patients on buprenorphine naloxone:
| Consideration | Description |
|---|---|
| Patient Assessment | A comprehensive assessment should be conducted to evaluate the patient’s medical history, current opioid use, and any co-occurring mental health conditions. |
| Dosage Adjustment | The initial dose of buprenorphine naloxone should be carefully titrated based on the patient’s individual needs and response. |
| Monitoring for Side Effects | Patients should be closely monitored for any potential side effects, including drowsiness, nausea, constipation, and withdrawal symptoms. |
| Drug Interactions | It is crucial to assess potential drug interactions with other medications the patient may be taking. |
| Behavioral Therapy | Behavioral therapies, such as cognitive-behavioral therapy (CBT) and contingency management, are essential for addressing underlying behavioral patterns and promoting long-term recovery. |
| Social Support | Encouraging patients to engage in social support networks and participate in recovery programs can significantly enhance treatment outcomes. |
| Relapse Prevention | Relapse prevention strategies should be implemented to help patients identify and manage triggers and develop coping mechanisms. |
| Long-Term Follow-Up | Regular follow-up appointments with a healthcare professional are crucial for monitoring progress, adjusting treatment plans, and addressing any emerging issues. |
Addressing Co-Occurring Mental Health Conditions
Co-occurring mental health conditions are prevalent among individuals with opioid use disorder, and addressing these conditions is essential for successful treatment. Mental health conditions can contribute to substance use and vice versa, creating a complex interplay that requires a comprehensive approach.
- Integrated Treatment: Integrating mental health treatment into opioid use disorder treatment is crucial for addressing both conditions simultaneously. This involves working with a multidisciplinary team of healthcare professionals, including psychiatrists, psychologists, and social workers.
- Psychosocial Interventions: Psychotherapy, such as CBT and dialectical behavior therapy (DBT), can help patients manage stress, develop coping skills, and address underlying mental health issues.
- Medication Management: If necessary, medications for mental health conditions, such as antidepressants or anti-anxiety medications, can be prescribed to manage symptoms and improve overall well-being.
Strategies for Promoting Long-Term Recovery from Opioid Addiction
Long-term recovery from opioid addiction is a continuous process that requires ongoing support and commitment. Here are some strategies for promoting sustained recovery:
- Sustained Medication Treatment: Continued medication treatment with buprenorphine naloxone or methadone can help prevent relapse and reduce cravings.
- Recovery Support Groups: Participating in recovery support groups, such as Narcotics Anonymous (NA) or SMART Recovery, can provide a sense of community, shared experiences, and ongoing support.
- Lifestyle Changes: Making healthy lifestyle changes, such as engaging in regular exercise, maintaining a balanced diet, and getting adequate sleep, can enhance overall well-being and contribute to recovery.
- Vocational Rehabilitation: Addressing employment-related challenges can help individuals regain a sense of purpose and financial stability, contributing to long-term recovery.
- Family and Social Support: Strong family and social support systems can play a crucial role in providing encouragement, accountability, and a sense of belonging during the recovery process.
Research and Development
Buprenorphine naloxone has been extensively studied, and ongoing research continues to provide valuable insights into its efficacy, safety, and potential applications. Recent research findings have reinforced its effectiveness as a medication-assisted treatment for opioid use disorder (OUD) and have shed light on its safety profile. However, further research is needed to explore specific aspects of its use and to optimize its potential benefits.
Efficacy and Safety
Numerous studies have demonstrated the efficacy of buprenorphine naloxone in treating OUD. Clinical trials have consistently shown that buprenorphine naloxone effectively reduces opioid cravings, withdrawal symptoms, and illicit opioid use. It has also been shown to improve patient retention in treatment and reduce the risk of overdose.
Regarding safety, buprenorphine naloxone is generally well-tolerated. The most common side effects are mild and often resolve on their own. However, serious adverse events, such as respiratory depression, are possible, particularly with high doses or in individuals with pre-existing respiratory conditions.
Areas for Further Research
Despite the substantial body of evidence supporting the use of buprenorphine naloxone, further research is warranted in several areas:
- Long-term efficacy and safety: More research is needed to understand the long-term effects of buprenorphine naloxone, particularly in individuals with chronic OUD.
- Optimal dosing strategies: Research is ongoing to determine the most effective dosing regimens for different patient populations, considering factors such as age, weight, and severity of OUD.
- Use in specific populations: Further research is needed to evaluate the safety and efficacy of buprenorphine naloxone in pregnant women, individuals with co-occurring mental health conditions, and those with chronic pain.
- Non-opioid addiction: Research is exploring the potential of buprenorphine naloxone for treating other addictions, such as alcohol use disorder and nicotine dependence.
Potential Future Applications
Buprenorphine naloxone’s potential applications extend beyond the treatment of OUD. Research is exploring its use in various settings:
- Emergency medical services: Buprenorphine naloxone has been investigated as a potential treatment for opioid overdose in prehospital settings.
- Pain management: Researchers are exploring the use of buprenorphine naloxone for chronic pain management, potentially reducing the risk of opioid dependence.
- Prevention of opioid misuse: Buprenorphine naloxone may have a role in preventing opioid misuse and addiction, particularly in individuals at high risk.
Legal and Regulatory Aspects
Buprenorphine naloxone, a medication used to treat opioid use disorder, is subject to strict legal and regulatory frameworks that aim to ensure its safe and effective use. These regulations address prescribing, dispensing, and monitoring of the medication, with a focus on preventing misuse and diversion.
Regulatory Agencies and Their Roles
Regulatory agencies play a crucial role in overseeing the safe and effective use of buprenorphine naloxone. The Food and Drug Administration (FDA) in the United States, for example, is responsible for approving the medication for its intended use and setting standards for its manufacturing and labeling.
The Drug Enforcement Administration (DEA) regulates the distribution and prescribing of buprenorphine naloxone, classifying it as a Schedule III controlled substance due to its potential for abuse. This classification means that the medication has a moderate to low potential for dependence and abuse compared to Schedule I or II drugs.
Prescription and Dispensing
Buprenorphine naloxone is available by prescription only, and its dispensing is subject to specific regulations. In the United States, healthcare providers must obtain a Data Waiver from the DEA to prescribe buprenorphine naloxone for opioid use disorder. This waiver allows providers to prescribe the medication to a limited number of patients, typically up to 100, and requires them to undergo training and certification in addiction medicine.
Availability and Accessibility
The availability and accessibility of buprenorphine naloxone vary depending on location and individual circumstances.
- Availability: Buprenorphine naloxone is generally available through pharmacies and other healthcare providers who are authorized to prescribe it.
- Accessibility: Factors that can influence accessibility include the availability of providers who are authorized to prescribe the medication, insurance coverage, and potential barriers related to stigma or cost.
Patient Monitoring and Reporting
To ensure the safe and effective use of buprenorphine naloxone, regulatory agencies often require patient monitoring and reporting. For instance, in the United States, the Prescription Drug Monitoring Program (PDMP) allows healthcare providers to access patient prescription history to prevent medication diversion and abuse.
Patient Perspectives and Experiences: Buprenorphine Naloxone
Buprenorphine naloxone, while a powerful tool for managing opioid use disorder, is experienced by each patient uniquely. Understanding these perspectives is crucial for tailoring treatment and providing effective support.
Patient Testimonials and Case Studies
Patient testimonials offer firsthand insights into the impact of buprenorphine naloxone treatment. These stories can highlight the challenges and benefits of using this medication, as well as the emotional journey of recovery.
“I was skeptical at first, but buprenorphine naloxone gave me the stability I needed to finally start rebuilding my life. I can now focus on work, my family, and my own well-being without being consumed by cravings.” – Sarah, a patient on buprenorphine naloxone treatment for 2 years.
Challenges and Benefits from a Patient’s Perspective
Patients on buprenorphine naloxone often face a range of challenges, including:
- Stigma and discrimination: The societal stigma associated with opioid use disorder can make it difficult for patients to seek help and feel comfortable disclosing their medication use.
- Side effects: While generally well-tolerated, buprenorphine naloxone can cause side effects such as nausea, constipation, and drowsiness. These side effects can be managed with proper medical guidance.
- Access to treatment: Finding a qualified provider and accessing affordable treatment can be challenging, particularly in areas with limited resources.
However, patients also report numerous benefits:
- Reduced cravings and withdrawal symptoms: Buprenorphine naloxone effectively reduces cravings and withdrawal symptoms, making it easier for patients to abstain from opioid use.
- Improved physical and mental health: With reduced opioid use, patients experience improved physical health, reduced risk of overdose, and improved mental well-being.
- Increased motivation and engagement in treatment: Buprenorphine naloxone allows patients to focus on other aspects of their lives, such as work, relationships, and hobbies, leading to increased motivation and engagement in treatment.
Resources and Support Systems
Patients on buprenorphine naloxone have access to various resources and support systems:
- Support groups: Connecting with others who have similar experiences can provide valuable support, understanding, and coping strategies.
- Therapy and counseling: Therapy can address underlying mental health issues, develop coping mechanisms, and build healthy life skills.
- Medication management programs: These programs provide ongoing monitoring and support, ensuring patients receive the appropriate medication dosage and address any potential side effects.
- Online resources and communities: Online platforms and communities offer information, support, and a sense of belonging for patients on buprenorphine naloxone.
Buprenorphine naloxone represents a significant advancement in the treatment of opioid use disorder. Its unique properties, including its partial agonist effect and the presence of naloxone, offer a safer and more effective alternative to traditional opioid substitution therapies. While ongoing research continues to refine our understanding of this medication, it has already proven to be a valuable tool in the fight against opioid addiction. As we move forward, it’s crucial to advocate for increased access to buprenorphine naloxone and to continue fostering a culture of compassion and understanding for individuals struggling with opioid addiction.
Buprenorphine naloxone is a medication often used for opioid use disorder, helping individuals manage withdrawal symptoms and cravings. While buprenorphine naloxone works on the opioid receptors, clonidine is another medication that can be helpful in managing withdrawal symptoms, specifically targeting the body’s blood pressure and heart rate. Both medications play crucial roles in supporting individuals through the process of recovery from opioid addiction.