Etanercept, a TNF-alpha inhibitor, has revolutionized the treatment of inflammatory diseases by targeting the root cause of inflammation. It works by blocking the signaling of tumor necrosis factor-alpha (TNF-alpha), a potent inflammatory protein that plays a central role in various autoimmune and inflammatory conditions.
By effectively inhibiting TNF-alpha, etanercept helps to manage symptoms, improve quality of life, and potentially even modify the course of these diseases. Its impact on patients with conditions like rheumatoid arthritis, psoriatic arthritis, and plaque psoriasis has been significant, offering hope for a better future.
Etanercept
Etanercept is a powerful medication used to treat a variety of inflammatory conditions. It is classified as a tumor necrosis factor-alpha (TNF-alpha) inhibitor, which means it works by blocking the action of TNF-alpha, a key protein involved in inflammation.
Mechanism of Action
Etanercept’s mechanism of action is based on its ability to bind to TNF-alpha, effectively preventing it from interacting with its receptors on cells. TNF-alpha is a pro-inflammatory cytokine, meaning it plays a crucial role in triggering and sustaining inflammatory responses. By inhibiting TNF-alpha, etanercept reduces inflammation and helps alleviate symptoms associated with various inflammatory diseases.
Role of TNF-alpha in Inflammatory Diseases
TNF-alpha is a central player in the development and progression of many inflammatory diseases. It contributes to inflammation by:
- Promoting the recruitment of immune cells to the site of inflammation.
- Stimulating the production of other inflammatory mediators.
- Inducing tissue damage.
By blocking TNF-alpha, etanercept helps to control these inflammatory processes and reduce the severity of symptoms.
Therapeutic Applications of Etanercept
Etanercept is a powerful biologic drug that has revolutionized the treatment of various inflammatory and autoimmune conditions. It works by targeting tumor necrosis factor (TNF), a key inflammatory protein that plays a crucial role in the development of these diseases. By blocking TNF, etanercept helps to reduce inflammation, alleviate symptoms, and improve the quality of life for patients.
Approved Indications for Etanercept
Etanercept is approved by the Food and Drug Administration (FDA) for the treatment of several autoimmune and inflammatory conditions. These include:
- Rheumatoid arthritis (RA)
- Psoriatic arthritis (PsA)
- Ankylosing spondylitis (AS)
- Plaque psoriasis
- Juvenile idiopathic arthritis (JIA)
Effectiveness of Etanercept in Managing Symptoms and Improving Quality of Life
Etanercept has been shown to be highly effective in managing symptoms and improving the quality of life for patients with various inflammatory conditions. In clinical trials, etanercept has been found to:
- Reduce joint pain and swelling
- Improve physical function
- Slow down the progression of joint damage
- Clear skin lesions in patients with psoriasis
- Reduce fatigue and improve overall well-being
Combination Therapies with Etanercept
Etanercept is often used in combination with other medications to enhance its effectiveness and manage specific patient needs. For example, in patients with rheumatoid arthritis, etanercept may be combined with:
- Methotrexate: A disease-modifying antirheumatic drug (DMARD) that slows the progression of RA
- Corticosteroids: Medications that reduce inflammation and suppress the immune system
- Other biologic therapies: Such as adalimumab or infliximab, which target TNF like etanercept
The combination of etanercept with other medications can provide a more comprehensive approach to managing inflammatory conditions and improve treatment outcomes for patients.
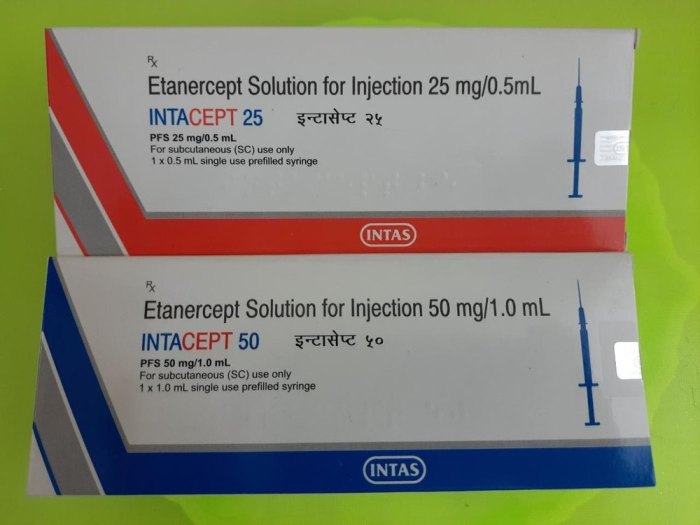
Administration and Dosage of Etanercept
Etanercept is administered by subcutaneous injection or intravenous infusion. The dosage regimen for etanercept depends on the specific indication and patient population. Factors such as patient weight, disease severity, and individual response can influence dosage adjustments.
Subcutaneous Administration
Etanercept is typically administered as a subcutaneous injection. The recommended dosage for various indications is as follows:
- Rheumatoid arthritis (RA): The usual starting dose is 50 mg administered subcutaneously once a week. The dosage may be increased to 50 mg twice a week based on individual response.
- Psoriatic arthritis (PsA): The usual starting dose is 50 mg administered subcutaneously once a week. The dosage may be increased to 50 mg twice a week based on individual response.
- Ankylosing spondylitis (AS): The usual starting dose is 50 mg administered subcutaneously once a week. The dosage may be increased to 50 mg twice a week based on individual response.
- Juvenile idiopathic arthritis (JIA): The recommended starting dose is 0.4 mg/kg administered subcutaneously once a week. The dosage may be adjusted based on individual response.
- Plaque psoriasis: The usual starting dose is 50 mg administered subcutaneously once a week. The dosage may be increased to 50 mg twice a week based on individual response.
Intravenous Administration
Etanercept can also be administered by intravenous infusion. The recommended dosage for various indications is as follows:
- Rheumatoid arthritis (RA): The usual starting dose is 25 mg administered intravenously once a week. The dosage may be increased to 25 mg twice a week based on individual response.
- Psoriatic arthritis (PsA): The usual starting dose is 25 mg administered intravenously once a week. The dosage may be increased to 25 mg twice a week based on individual response.
- Ankylosing spondylitis (AS): The usual starting dose is 25 mg administered intravenously once a week. The dosage may be increased to 25 mg twice a week based on individual response.
- Juvenile idiopathic arthritis (JIA): The recommended starting dose is 0.4 mg/kg administered intravenously once a week. The dosage may be adjusted based on individual response.
- Plaque psoriasis: The usual starting dose is 25 mg administered intravenously once a week. The dosage may be increased to 25 mg twice a week based on individual response.
Dosage Adjustments
Dosage adjustments may be necessary based on factors such as patient weight, disease severity, and individual response.
- Patient weight: In patients with a body weight less than 50 kg, the starting dose may be reduced. For patients with a body weight greater than 100 kg, the starting dose may be increased.
- Disease severity: In patients with severe disease, the starting dose may be increased. In patients with mild disease, the starting dose may be reduced.
- Individual response: If the patient does not respond to the initial dosage, the dosage may be increased. If the patient experiences side effects, the dosage may be reduced.
Pharmacokinetics and Metabolism of Etanercept
Etanercept’s pharmacokinetic profile governs its absorption, distribution, metabolism, and elimination in the body. Understanding these processes is crucial for determining appropriate dosing regimens and predicting potential drug interactions.
Absorption and Distribution
Etanercept is administered subcutaneously, and its absorption is generally rapid and complete. Once absorbed, etanercept distributes throughout the body, primarily binding to its target, tumor necrosis factor-alpha (TNF-α). This binding is highly specific, resulting in a long half-life and prolonged therapeutic effect.
Metabolism and Elimination
Etanercept is not metabolized in the body. It is eliminated primarily through catabolism, where it is broken down into smaller fragments. These fragments are then cleared from the body through the kidneys and feces.
Half-Life and Dosing Frequency
Etanercept has a long half-life, typically ranging from 7 to 14 days. This prolonged half-life allows for infrequent dosing, usually once or twice weekly, depending on the specific indication and patient response. The long half-life minimizes the need for frequent injections, improving patient convenience and adherence to treatment.
Potential for Drug Interactions
Etanercept has the potential to interact with other medications, particularly those that affect the immune system. These interactions can lead to increased risk of infections or other adverse effects. For example, etanercept may increase the risk of infections when used concurrently with other immunosuppressants or with live vaccines. Therefore, it is essential to carefully consider the potential for drug interactions before initiating etanercept therapy.
Safety and Adverse Effects of Etanercept
Etanercept, like other TNF inhibitors, can cause a range of adverse effects, some of which can be serious. Understanding these potential risks is crucial for safe and effective treatment. This section will discuss common and serious adverse effects, including the risk of infections, hypersensitivity reactions, and other immune-mediated adverse events.
Infections
Infections are a significant concern with etanercept therapy due to its immunosuppressive properties. Etanercept can increase the risk of developing infections, including both common and serious infections.
- Common infections: Upper respiratory tract infections, such as colds and sinusitis, are commonly reported. Other common infections include skin infections, urinary tract infections, and gastrointestinal infections.
- Serious infections: Etanercept can increase the risk of developing serious infections, such as tuberculosis, pneumonia, sepsis, and fungal infections. These infections can be life-threatening.
It is essential to carefully assess the risk of infections before starting etanercept therapy. Patients with a history of infections, particularly tuberculosis, should be closely monitored.
Risk of Tuberculosis
Etanercept can reactivate latent tuberculosis infection. Before initiating etanercept therapy, it is essential to assess the risk of latent tuberculosis infection and perform appropriate screening tests. If latent tuberculosis is detected, treatment with anti-tuberculosis medication should be initiated before starting etanercept.
Opportunistic Infections
Etanercept can increase the risk of developing opportunistic infections, which are infections caused by organisms that usually do not cause disease in people with healthy immune systems.
- Fungal infections: Etanercept can increase the risk of developing fungal infections, such as candidiasis (yeast infection) and aspergillosis.
- Viral infections: Etanercept can increase the risk of developing viral infections, such as cytomegalovirus (CMV) and herpes simplex virus (HSV).
- Parasitic infections: Etanercept can increase the risk of developing parasitic infections, such as toxoplasmosis and cryptosporidiosis.
Hypersensitivity Reactions
Etanercept can cause hypersensitivity reactions, which are allergic reactions. These reactions can range from mild to severe.
- Mild reactions: Mild hypersensitivity reactions may include rash, itching, and hives.
- Severe reactions: Severe hypersensitivity reactions can include anaphylaxis, a life-threatening allergic reaction that can cause difficulty breathing, swelling of the face and throat, and a drop in blood pressure.
Other Immune-Mediated Adverse Events
Etanercept can also cause other immune-mediated adverse events, such as autoimmune disorders. These disorders can affect various organs, including the liver, kidneys, and nervous system.
- Hepatitis: Etanercept can cause hepatitis, inflammation of the liver.
- Nephritis: Etanercept can cause nephritis, inflammation of the kidneys.
- Neurological disorders: Etanercept can cause neurological disorders, such as multiple sclerosis (MS) and Guillain-Barré syndrome (GBS).
Monitoring and Management of Etanercept Therapy
Etanercept therapy, like any medication, requires careful monitoring to ensure its effectiveness and safety. Regular assessments are crucial for identifying potential adverse effects, evaluating disease activity, and making informed decisions about treatment adjustments.
Importance of Regular Monitoring
Regular monitoring is essential for detecting early signs of adverse effects and disease activity. This allows for timely interventions to minimize potential complications and optimize treatment outcomes.
- Adverse Effects: Monitoring for adverse effects, such as infections, allergic reactions, and autoimmune disorders, is crucial. Early detection allows for prompt management and may prevent serious complications.
- Disease Activity: Monitoring disease activity is equally important to assess the effectiveness of etanercept therapy. This involves evaluating clinical symptoms, laboratory markers, and imaging studies to determine if the treatment is achieving its desired goals.
Laboratory Tests
Laboratory tests play a vital role in monitoring etanercept therapy. They provide valuable insights into potential adverse effects and disease activity.
- Complete Blood Count (CBC): CBC helps monitor for anemia, leukopenia (low white blood cell count), and thrombocytopenia (low platelet count), which can be associated with etanercept therapy.
- Liver Function Tests (LFTs): LFTs are used to assess liver function, as etanercept can potentially affect liver enzymes. Elevated liver enzymes may indicate liver damage and require further investigation.
Patient Education and Counseling
Patient education and counseling are essential components of etanercept therapy management. They empower patients to actively participate in their care and make informed decisions about their treatment.
- Understanding Etanercept: Patients should be educated about the mechanism of action, potential benefits, and risks associated with etanercept therapy.
- Monitoring for Adverse Effects: Patients should be instructed on how to monitor for potential adverse effects and report any unusual symptoms to their healthcare provider.
- Compliance with Treatment: Patients should be counseled on the importance of adhering to their prescribed dosage and schedule to ensure optimal treatment outcomes.
Etanercept in Clinical Trials and Research
Etanercept has been extensively studied in numerous clinical trials, demonstrating its efficacy and safety in treating various inflammatory conditions. Ongoing research continues to explore its potential in other diseases, and novel formulations are being developed to enhance its therapeutic profile.
Efficacy and Safety in Clinical Trials
Etanercept has shown remarkable efficacy in treating various inflammatory conditions, including rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, plaque psoriasis, and juvenile idiopathic arthritis.
- In rheumatoid arthritis, etanercept has been shown to reduce joint inflammation, pain, and stiffness, improving functional capacity and quality of life. It has also been found to delay joint damage and prevent disease progression.
- In psoriatic arthritis, etanercept effectively alleviates joint pain, swelling, and skin lesions, improving physical function and overall well-being.
- In ankylosing spondylitis, etanercept reduces spinal inflammation, pain, and stiffness, leading to improved mobility and reduced disability.
- In plaque psoriasis, etanercept significantly clears skin lesions, improving skin appearance and quality of life.
- In juvenile idiopathic arthritis, etanercept effectively manages joint inflammation and pain, promoting normal growth and development.
Etanercept has a generally favorable safety profile, with the most common side effects being injection site reactions, upper respiratory tract infections, and headache. Serious adverse events are relatively rare, but they can occur, including infections, allergic reactions, and autoimmune disorders.
Ongoing Research and Potential Applications
Ongoing research is investigating the potential use of etanercept in other inflammatory conditions, such as Crohn’s disease, ulcerative colitis, and systemic lupus erythematosus.
- In Crohn’s disease and ulcerative colitis, etanercept is being explored as a potential treatment for reducing inflammation and improving symptoms in patients with moderate to severe disease.
- In systemic lupus erythematosus, etanercept is being investigated for its ability to suppress the autoimmune response and reduce inflammation.
Future Directions for Etanercept Research
Future research on etanercept focuses on developing novel formulations and targeted delivery approaches to enhance its therapeutic efficacy and safety.
- Researchers are exploring the development of long-acting etanercept formulations, which would require less frequent injections and potentially improve patient adherence.
- Targeted delivery approaches are being investigated to deliver etanercept directly to the site of inflammation, reducing systemic exposure and minimizing side effects.
Etanercept and Patient Perspectives
Etanercept treatment can have a significant impact on patients’ lives, offering relief from the debilitating symptoms of autoimmune diseases. Understanding the experiences and perspectives of patients who have undergone etanercept therapy is crucial for appreciating its true value and navigating the challenges that may arise.
Patient Testimonials and Experiences
Patient testimonials provide valuable insights into the real-world impact of etanercept treatment. These stories highlight the diverse ways in which etanercept can improve patients’ lives, from reducing pain and inflammation to enhancing mobility and overall well-being.
“Before starting etanercept, I couldn’t walk for more than a few minutes without excruciating pain. Now, I can go for walks in the park with my family. It’s changed my life.” – Sarah, a patient with rheumatoid arthritis.
“Etanercept has given me back my independence. I used to be constantly tired and in pain, but now I can participate in activities I love, like gardening and spending time with my grandchildren.” – John, a patient with psoriatic arthritis.
Impact of Etanercept on Patients’ Lives
Etanercept treatment can significantly improve various aspects of patients’ lives, including:
- Physical Function: Etanercept can reduce joint pain and inflammation, leading to improved mobility and physical function. Patients may experience increased range of motion, decreased stiffness, and the ability to perform daily activities with greater ease.
- Pain Relief: Etanercept can effectively manage pain associated with autoimmune diseases, allowing patients to experience significant pain reduction and improved quality of life. This can lead to a decrease in the need for pain medication and increased participation in social and recreational activities.
- Overall Well-being: Etanercept can improve patients’ overall well-being by reducing fatigue, improving sleep quality, and enhancing mood. These improvements can have a positive impact on patients’ mental health and emotional well-being, leading to a greater sense of satisfaction with life.
Challenges and Concerns During Etanercept Therapy
While etanercept offers significant benefits, patients may face certain challenges and concerns during therapy:
- Injection Site Reactions: Some patients may experience injection site reactions, such as redness, pain, or swelling. These reactions are usually mild and can be managed with over-the-counter medications or by changing the injection site.
- Infections: Etanercept can suppress the immune system, increasing the risk of infections. Patients should be aware of the signs and symptoms of infection and seek medical attention promptly if they develop any concerns.
- Cost: Etanercept can be expensive, and patients may face challenges accessing the medication due to insurance coverage limitations or high out-of-pocket costs.
- Long-Term Effects: The long-term effects of etanercept are still being studied. Patients should discuss any concerns about potential long-term effects with their healthcare provider.
Comparison of Etanercept to Other TNF-alpha Inhibitors

Etanercept, infliximab, and adalimumab are all TNF-alpha inhibitors used to treat various inflammatory conditions, including rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and Crohn’s disease. While they share the same mechanism of action, there are differences in their efficacy, safety, and pharmacokinetic profiles.
Efficacy
The efficacy of TNF-alpha inhibitors varies depending on the specific condition and patient characteristics.
- Etanercept, infliximab, and adalimumab have all demonstrated efficacy in clinical trials for rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and Crohn’s disease.
- In rheumatoid arthritis, all three drugs have been shown to improve joint pain, swelling, and function. However, head-to-head studies comparing their efficacy have shown mixed results.
- In Crohn’s disease, infliximab may be slightly more effective than etanercept in inducing remission.
- In psoriasis, etanercept and adalimumab have demonstrated similar efficacy in achieving clear or almost clear skin.
Safety
The safety profiles of TNF-alpha inhibitors are generally similar, with the most common adverse effects being infections, infusion reactions, and injection site reactions.
- Infliximab has a higher risk of infusion reactions, which can be serious and even life-threatening.
- Etanercept and adalimumab are administered subcutaneously, which reduces the risk of infusion reactions.
- All TNF-alpha inhibitors increase the risk of infections, including tuberculosis, opportunistic infections, and serious bacterial infections.
- TNF-alpha inhibitors are associated with an increased risk of lymphoma and other malignancies, but the absolute risk is still low.
Pharmacokinetics
Etanercept, infliximab, and adalimumab have different pharmacokinetic profiles.
- Etanercept is a fusion protein with a longer half-life than infliximab or adalimumab. This means that it is administered less frequently.
- Infliximab is a monoclonal antibody that is administered intravenously.
- Adalimumab is a monoclonal antibody that is administered subcutaneously.
Factors Influencing TNF-alpha Inhibitor Choice
The choice of a specific TNF-alpha inhibitor for a particular patient is based on several factors, including:
- The specific disease being treated
- The patient’s medical history and risk factors
- The patient’s preference for administration route and frequency
- The cost of the medication
Advantages and Disadvantages
- Etanercept
- Advantages: Longer half-life, subcutaneous administration, lower risk of infusion reactions.
- Disadvantages: May be less effective than infliximab in Crohn’s disease, higher cost.
- Infliximab
- Advantages: May be more effective than etanercept in Crohn’s disease, lower cost.
- Disadvantages: Higher risk of infusion reactions, intravenous administration, shorter half-life.
- Adalimumab
- Advantages: Subcutaneous administration, longer half-life than infliximab, lower risk of infusion reactions.
- Disadvantages: Higher cost than etanercept, may be less effective than infliximab in Crohn’s disease.
Etanercept and Biosimilar Medications
Biosimilar medications are biological products that are highly similar to an already approved, original biologic product, known as the reference product. These biosimilars are designed to provide safe and effective alternatives to the original biologics, often at a lower cost.
Development and Approval Process for Etanercept Biosimilars
The development and approval process for etanercept biosimilars involves rigorous scientific and regulatory scrutiny to ensure they meet the same high standards as the original product.
- Extensive Preclinical Studies: Biosimilar developers conduct comprehensive preclinical studies to demonstrate that the biosimilar has a similar structure, function, and mechanism of action as the reference product.
- Clinical Trials: Clinical trials are essential for demonstrating the efficacy, safety, and immunogenicity of the biosimilar. These trials involve comparing the biosimilar to the reference product in patients with the same disease.
- Regulatory Review: Biosimilar applications are reviewed by regulatory agencies, such as the FDA in the United States, to ensure that the biosimilar is highly similar to the reference product in terms of quality, safety, and efficacy. This review includes a thorough assessment of the biosimilar’s manufacturing process, analytical data, and clinical trial results.
Efficacy, Safety, and Interchangeability of Etanercept Biosimilars
Numerous studies have demonstrated that etanercept biosimilars are highly similar to the original etanercept product in terms of efficacy, safety, and immunogenicity.
- Efficacy: Clinical trials have shown that etanercept biosimilars are as effective as the original etanercept in treating conditions such as rheumatoid arthritis, psoriatic arthritis, and plaque psoriasis.
- Safety: Safety profiles of etanercept biosimilars are comparable to the original product. Side effects observed with biosimilars are generally consistent with the known safety profile of etanercept.
- Interchangeability: In some countries, etanercept biosimilars have been deemed interchangeable with the original etanercept. This means that pharmacists can substitute a biosimilar for the original product without the need for a physician’s approval.
“Biosimilar medications offer a valuable option for patients who need access to biologic therapies but may face financial constraints. By providing affordable alternatives to originator biologics, biosimilars can help improve patient access to these important treatments.”
Etanercept and the Future of Inflammatory Disease Management
The treatment landscape for inflammatory diseases is continuously evolving, with biologic therapies like etanercept playing a pivotal role in managing these conditions. Etanercept, a TNF-alpha inhibitor, has revolutionized the treatment of inflammatory diseases, offering effective relief and improved quality of life for many patients. As research progresses, the future of inflammatory disease management promises even more personalized and targeted therapies.
Personalized Medicine and Targeted Therapies
Personalized medicine aims to tailor treatments to individual patients based on their unique genetic and biological characteristics. This approach has the potential to optimize treatment outcomes and minimize side effects. In the context of inflammatory diseases, personalized medicine is being explored through:
- Genetic testing: Identifying specific genetic markers associated with disease susceptibility and response to different therapies can help clinicians select the most appropriate treatment for each patient. For example, genetic testing can help predict the likelihood of developing certain inflammatory diseases, such as rheumatoid arthritis, and can guide the choice of treatment.
- Biomarker analysis: Monitoring specific biomarkers in the blood or other bodily fluids can provide insights into disease activity and response to therapy. This allows for personalized adjustments to treatment regimens, ensuring optimal efficacy and minimizing the risk of adverse effects.
- Immunotherapy: This approach focuses on modulating the immune system to target specific inflammatory pathways. Emerging immunotherapies, such as chimeric antigen receptor (CAR) T-cell therapy, show promise in treating various inflammatory conditions, offering the potential for long-term disease remission.
Future Directions for Etanercept Development
Etanercept’s future development is driven by ongoing research and clinical trials, aiming to:
- Improve efficacy and safety: Research is ongoing to optimize etanercept’s efficacy and minimize side effects. This may involve exploring different formulations, delivery methods, and combination therapies.
- Expand therapeutic applications: Etanercept’s therapeutic potential extends beyond its current approved indications. Ongoing research is investigating its effectiveness in treating other inflammatory conditions, such as inflammatory bowel disease and psoriasis.
- Develop long-acting formulations: Developing long-acting formulations of etanercept could reduce the frequency of injections, improving patient convenience and adherence to therapy.
Impact on Patient Care
The future of etanercept and other biologic therapies holds significant promise for improving patient care in inflammatory disease management. These advancements have the potential to:
- Reduce disease burden: More effective and targeted therapies can help reduce the symptoms, severity, and long-term complications associated with inflammatory diseases.
- Enhance quality of life: Improved treatment options can lead to greater functional capacity, reduced pain and inflammation, and overall better well-being for patients.
- Reduce healthcare costs: By optimizing treatment outcomes and minimizing the need for hospitalizations and other costly interventions, personalized and targeted therapies can potentially reduce healthcare costs associated with inflammatory diseases.
Etanercept represents a remarkable advancement in the treatment of inflammatory diseases. Its ability to effectively target TNF-alpha has led to significant improvements in symptom management and quality of life for countless patients. As research continues, we can anticipate further advancements in understanding and treating inflammatory diseases, potentially leading to even more effective and targeted therapies.
Etanercept is a medication commonly used to treat autoimmune diseases like rheumatoid arthritis. While it primarily targets the immune system, it’s important to remember that it’s not a cure-all. For those also managing cardiovascular health, it’s crucial to consult with a healthcare professional about potential interactions with medications like effient , a drug often prescribed to prevent blood clots.
This ensures the safest and most effective treatment plan for your specific needs.