Ipratropium, a widely used anticholinergic bronchodilator, plays a crucial role in managing various respiratory conditions. This medication works by relaxing the muscles in the airways, opening them up and easing breathing. It’s available in different formulations, including nasal sprays and inhalers, offering flexibility for patients with varying needs.
From treating chronic obstructive pulmonary disease (COPD) and asthma to managing rhinitis symptoms, ipratropium offers relief from wheezing, shortness of breath, and coughing. Its effectiveness and safety profile have made it a cornerstone in the treatment of respiratory illnesses, improving the quality of life for millions of individuals worldwide.
Ipratropium

Ipratropium bromide is a medication that is used to treat the symptoms of chronic obstructive pulmonary disease (COPD) and asthma. It is a type of medication known as an anticholinergic bronchodilator.
Chemical Structure and Properties
Ipratropium is a synthetic compound that is structurally similar to the naturally occurring neurotransmitter acetylcholine. It has a quaternary ammonium structure, which means that it carries a positive charge. This positive charge is important for its interaction with the muscarinic receptors in the lungs. Ipratropium is a white, crystalline powder that is soluble in water. It is available as a solution for inhalation, nasal spray, and injection.
Mechanism of Action
Ipratropium works by blocking the action of acetylcholine at muscarinic receptors in the lungs. Acetylcholine is a neurotransmitter that causes bronchoconstriction, or narrowing of the airways. By blocking the action of acetylcholine, ipratropium helps to relax the muscles in the airways and open them up. This allows for easier breathing.
Formulations
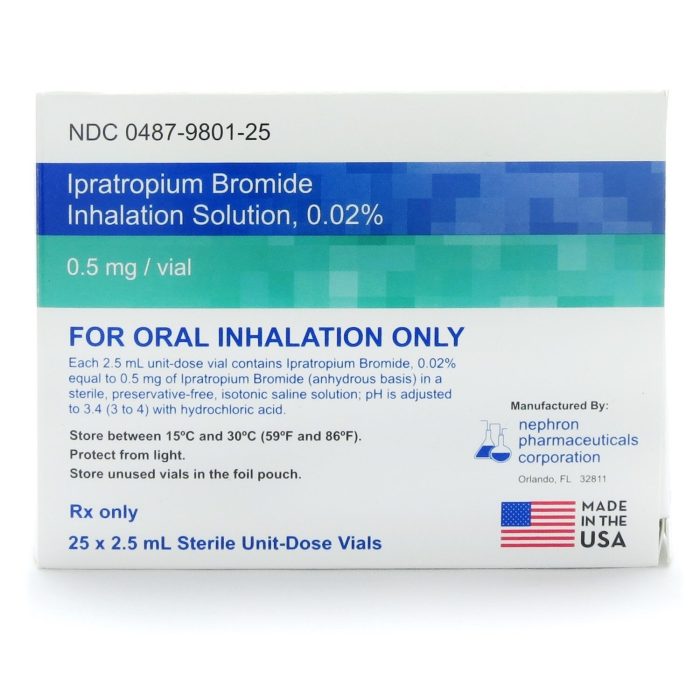
Ipratropium is available in several different formulations, including:
- Inhalation solutions: Ipratropium inhalation solutions are the most common formulation of ipratropium. They are available in metered-dose inhalers (MDIs), nebulizers, and dry powder inhalers (DPIs). MDIs are small, handheld devices that deliver a measured dose of medication to the lungs. Nebulizers are devices that convert liquid medication into a fine mist that can be inhaled. DPIs are devices that contain a powder that is inhaled into the lungs.
- Nasal spray: Ipratropium nasal spray is used to treat the symptoms of rhinitis, which is inflammation of the nasal passages.
- Injection: Ipratropium injection is used to treat bronchospasm, or narrowing of the airways, in patients who are unable to use inhaled medications.
Therapeutic Applications of Ipratropium
Ipratropium is a medication that belongs to a class of drugs known as anticholinergics. It works by blocking the action of acetylcholine, a neurotransmitter that causes the muscles in the airways to contract. By relaxing these muscles, ipratropium helps to open up the airways and make it easier to breathe.
Ipratropium is primarily used to treat respiratory conditions that cause bronchospasm, or narrowing of the airways. These conditions include chronic obstructive pulmonary disease (COPD), asthma, and rhinitis.
Treatment of COPD
COPD is a chronic lung disease that causes airflow obstruction and shortness of breath. It is often caused by smoking or exposure to other irritants. Ipratropium is a mainstay treatment for COPD, helping to improve lung function and reduce symptoms like wheezing, shortness of breath, and coughing. It is often used in combination with other medications, such as inhaled corticosteroids, to manage the disease effectively.
Treatment of Asthma
Asthma is a chronic inflammatory disease of the airways that causes wheezing, shortness of breath, chest tightness, and coughing. Ipratropium is used to treat asthma, especially in patients who experience bronchospasm, particularly those with mild to moderate asthma. It is often used as a rescue inhaler for sudden asthma attacks.
Treatment of Rhinitis
Rhinitis is an inflammation of the nasal passages that causes nasal congestion, runny nose, sneezing, and itching. Ipratropium is available as a nasal spray to treat allergic rhinitis, also known as hay fever. It helps to reduce nasal congestion and other symptoms by blocking the action of acetylcholine in the nasal passages.
Comparison with Other Bronchodilators
Ipratropium is a long-acting bronchodilator, meaning that it provides relief from bronchospasm for several hours. It is often compared to other bronchodilators, such as albuterol, which is a short-acting bronchodilator.
Strengths of Ipratropium
- Provides long-lasting relief from bronchospasm.
- Has fewer side effects than some other bronchodilators.
- Can be used to treat both COPD and asthma.
Limitations of Ipratropium
- May not be as effective as other bronchodilators in treating severe bronchospasm.
- Can take some time to work, making it less effective for acute attacks.
- Not suitable for everyone, as it can cause side effects such as dry mouth, headache, and blurred vision.
Pharmacokinetics and Metabolism of Ipratropium

Ipratropium’s pharmacokinetic profile encompasses its absorption, distribution, metabolism, and excretion within the body. Understanding these processes is crucial for optimizing its therapeutic efficacy and minimizing potential adverse effects.
Absorption, Ipratropium
Ipratropium is primarily administered via inhalation, delivering the drug directly to the respiratory tract. This route of administration offers several advantages, including a rapid onset of action and a reduced systemic exposure to the drug, minimizing potential side effects.
Distribution
Once absorbed, ipratropium distributes to various tissues, including the lungs, where it exerts its bronchodilator effects. However, its distribution is limited by its high molecular weight and hydrophilic nature, which restrict its penetration across cell membranes. Consequently, ipratropium exhibits low systemic bioavailability, meaning that only a small portion of the inhaled dose reaches the bloodstream.
Metabolism
Ipratropium undergoes significant metabolism in the liver, primarily through hydrolysis and oxidation. The primary metabolite, a less active compound, is excreted in urine.
Excretion
Ipratropium and its metabolites are primarily eliminated through the kidneys. Excretion is primarily through urine, with a smaller amount excreted in feces. The elimination half-life of ipratropium is approximately 6 to 8 hours.
Factors Influencing Pharmacokinetics
Several factors can influence ipratropium’s pharmacokinetic profile, including:
Dosage
The dosage of ipratropium directly affects its plasma concentration and duration of action. Higher doses generally result in higher plasma levels and a longer duration of effect.
Route of Administration
Inhalation is the preferred route of administration for ipratropium, as it delivers the drug directly to the lungs, maximizing its therapeutic effect and minimizing systemic exposure.
Patient Characteristics
Patient characteristics, such as age, renal function, and hepatic function, can influence ipratropium’s pharmacokinetic profile. For instance, individuals with impaired renal function may experience reduced drug clearance and increased plasma concentrations.
Drug Interactions
Ipratropium has a low potential for drug interactions due to its limited systemic bioavailability. However, potential interactions may occur with other medications that affect the same metabolic pathways or target similar receptors.
Safety and Adverse Effects of Ipratropium
Ipratropium is generally well-tolerated, but like all medications, it can cause side effects. Most adverse effects are mild and transient, but some can be serious. It’s important to be aware of the potential risks associated with ipratropium use, especially for specific patient populations.
Common and Rare Adverse Effects of Ipratropium
The most common adverse effects of ipratropium are related to its anticholinergic properties, which block the action of acetylcholine, a neurotransmitter involved in various bodily functions. These effects can include:
- Dry mouth: This is the most frequent side effect, occurring in about 10% of patients. It’s usually mild and resolves on its own.
- Blurred vision: This is also a common side effect, affecting around 5% of patients. It’s usually temporary and resolves within a few hours.
- Urinary retention: This is a less common side effect, affecting about 1% of patients. It can be more pronounced in individuals with pre-existing urinary problems.
- Constipation: This can occur in some patients, especially those with pre-existing constipation.
- Headache: This is a relatively common side effect, occurring in about 5% of patients.
- Dizziness: This can occur in some patients, especially when starting treatment.
- Tremor: This is a rare side effect, occurring in less than 1% of patients.
- Bronchospasm: This is a paradoxical effect, meaning it’s the opposite of the intended effect. It’s rare, but it can occur in some patients, especially those with a history of asthma.
Potential Risks of Ipratropium Use in Specific Patient Populations
- Pregnant women: Ipratropium is classified as pregnancy category C, meaning that animal studies have shown adverse effects on the fetus, but there are no adequate and well-controlled studies in humans. The potential benefits of using ipratropium in pregnant women must be weighed against the potential risks.
- Nursing mothers: Ipratropium is excreted in breast milk, but the amount is generally considered to be low and unlikely to cause harm to the infant. However, it’s important to discuss the risks and benefits with a healthcare professional before using ipratropium while breastfeeding.
- Individuals with certain medical conditions: Ipratropium should be used with caution in individuals with certain medical conditions, such as:
- Prostatic hypertrophy: This condition can increase the risk of urinary retention.
- Glaucoma: This condition can be exacerbated by ipratropium.
- Myasthenia gravis: This condition can be worsened by ipratropium.
- Cardiovascular disease: Ipratropium can increase heart rate and blood pressure.
Adverse Effects Table
| Effect | Frequency | Severity | Management |
|---|---|---|---|
| Dry mouth | Common | Mild | Usually resolves on its own. Sip on water or sugar-free candy. |
| Blurred vision | Common | Mild | Usually resolves within a few hours. Avoid driving or operating machinery until vision clears. |
| Urinary retention | Uncommon | Moderate | Contact healthcare provider if symptoms persist. |
| Constipation | Uncommon | Mild | Increase fiber intake and fluid intake. |
| Headache | Common | Mild | Usually resolves on its own. Over-the-counter pain relievers can be used. |
| Dizziness | Common | Mild | Avoid activities that require alertness until dizziness subsides. |
| Tremor | Rare | Mild | Usually resolves on its own. |
| Bronchospasm | Rare | Severe | Discontinue ipratropium and seek immediate medical attention. |
Ipratropium in Clinical Practice
Ipratropium is a widely used medication for treating respiratory conditions, particularly those characterized by bronchospasm. Its effectiveness and safety profile make it a valuable tool in clinical practice, but understanding appropriate dosage regimens, monitoring guidelines, and patient education is crucial for maximizing therapeutic benefits and minimizing potential adverse effects.
Dosage Regimens
Dosage regimens for ipratropium vary depending on the specific medical setting, the severity of the condition, and the patient’s individual needs.
- Acute Exacerbations: In cases of acute exacerbations of chronic obstructive pulmonary disease (COPD) or asthma, ipratropium is typically administered via inhalation as a nebulizer solution. The initial dose is usually 0.5 mg, followed by additional doses as needed, up to a maximum of 4 mg per day.
- Long-Term Maintenance Therapy: For long-term maintenance therapy of COPD, ipratropium is often used in conjunction with other medications, such as inhaled corticosteroids. The usual dosage is 2 inhalations (18 mcg each) twice daily.
- Other Settings: In settings such as cystic fibrosis, ipratropium may be used in conjunction with other therapies to improve lung function.
Monitoring Patients Receiving Ipratropium Treatment
Regular monitoring is essential to ensure the effectiveness and safety of ipratropium treatment.
- Lung Function Tests: Monitoring lung function with tests such as spirometry is crucial to assess the response to treatment and detect any deterioration.
- Heart Rate and Blood Pressure: Ipratropium can cause an increase in heart rate and blood pressure, so monitoring these vital signs is important, especially in patients with pre-existing cardiovascular conditions.
- Adverse Effects: Patients should be closely monitored for any signs of adverse effects, such as dry mouth, cough, or urinary retention.
Patient Education and Adherence
Patient education is essential for ensuring adherence to treatment plans and maximizing the benefits of ipratropium therapy.
- Proper Inhaler Technique: Patients should be instructed on the correct technique for using inhalers to ensure optimal drug delivery to the lungs.
- Importance of Regular Use: Patients should understand the importance of taking ipratropium regularly, even when they are feeling well, to prevent exacerbations.
- Potential Adverse Effects: Patients should be informed about potential adverse effects and instructed to report any unusual symptoms to their healthcare provider.
Research and Development of Ipratropium
While ipratropium has been a mainstay in the treatment of respiratory conditions for decades, ongoing research continues to explore its potential and refine its application. Current research efforts focus on developing new formulations, investigating its use in other respiratory conditions, and optimizing its safety and efficacy.
New Formulations and Combination Therapies
The development of new formulations is a significant area of research, aiming to enhance the delivery, efficacy, and convenience of ipratropium therapy.
- Long-acting formulations: Researchers are exploring long-acting formulations of ipratropium, potentially reducing the frequency of administration and improving patient adherence. These formulations aim to provide sustained bronchodilation for extended periods, offering greater convenience for patients.
- Combination therapies: Ipratropium is increasingly being combined with other medications, such as inhaled corticosteroids, to achieve a synergistic effect in managing respiratory conditions. This approach aims to address multiple aspects of the disease process, potentially improving patient outcomes.
Ipratropium in Other Respiratory Conditions
Ipratropium’s potential application in other respiratory conditions beyond asthma and COPD is being investigated.
- Chronic obstructive pulmonary disease (COPD): Ipratropium is a cornerstone treatment for COPD, but research continues to explore its use in specific subtypes of COPD and in managing exacerbations.
- Cystic fibrosis: Ipratropium’s bronchodilatory effects have shown promise in treating airway obstruction in cystic fibrosis patients, leading to further research on its efficacy and safety in this population.
- Bronchiectasis: Research is exploring the potential of ipratropium in managing airway inflammation and mucus hypersecretion in bronchiectasis, a chronic lung disease characterized by airway dilation and recurrent infections.
Optimizing Safety and Efficacy
Research efforts are dedicated to optimizing the safety and efficacy of ipratropium therapy.
- Dose optimization: Researchers are investigating optimal dosing strategies to maximize therapeutic benefits while minimizing potential side effects. This includes exploring personalized dosing regimens based on patient characteristics and disease severity.
- Drug interactions: Studies are conducted to identify potential drug interactions with ipratropium, aiming to ensure safe and effective use in combination therapies. This includes evaluating the potential for ipratropium to interact with other medications commonly used in respiratory care.
- Long-term safety: Ongoing research focuses on evaluating the long-term safety profile of ipratropium, particularly in vulnerable populations such as children and the elderly. This includes monitoring for potential adverse effects and assessing the risk-benefit profile over extended periods of use.
Ipratropium and Patient Education
Ipratropium is a medication that helps to open up the airways in your lungs. It is used to treat chronic obstructive pulmonary disease (COPD) and asthma. This leaflet will explain the purpose, proper use, and potential side effects of ipratropium.
Understanding Ipratropium
Ipratropium is a type of medication called an anticholinergic. It works by blocking the action of a chemical in your body called acetylcholine. Acetylcholine causes your airways to narrow. By blocking acetylcholine, ipratropium helps to relax the muscles in your airways, making it easier to breathe.
Using Ipratropium Safely and Effectively
- Always follow your doctor’s instructions carefully when using ipratropium.
- Use the inhaler exactly as your doctor prescribes.
- Do not use more ipratropium than your doctor recommends.
- Do not stop using ipratropium without talking to your doctor first.
- Keep ipratropium out of reach of children and pets.
Potential Side Effects of Ipratropium
Like all medications, ipratropium can cause side effects. Some common side effects include:
- Dry mouth
- Cough
- Sore throat
- Headache
If you experience any of these side effects, they usually go away on their own. However, if they are severe or persistent, talk to your doctor.
Questions to Ask Your Healthcare Provider
Patients should ask their healthcare providers about ipratropium treatment. Here are some questions to consider:
- How often should I use ipratropium?
- How long will I need to take ipratropium?
- What are the potential side effects of ipratropium?
- Are there any foods or drinks I should avoid while taking ipratropium?
- What should I do if I miss a dose of ipratropium?
- What are the long-term effects of ipratropium?
- What are the signs of an allergic reaction to ipratropium?
- What other medications can interact with ipratropium?
- Is there a generic version of ipratropium available?
Managing Common Side Effects
- To manage dry mouth, drink plenty of water or sugar-free liquids.
- To manage cough, try sucking on cough drops or using a humidifier.
- To manage sore throat, gargle with salt water or use lozenges.
- To manage headache, take over-the-counter pain relievers such as ibuprofen or acetaminophen.
Ipratropium and Public Health
Ipratropium plays a vital role in improving public health by effectively managing chronic respiratory diseases, such as chronic obstructive pulmonary disease (COPD) and asthma. By understanding the role of ipratropium in these conditions, we can better address the public health challenges associated with respiratory illnesses.
Early Diagnosis and Treatment
Early diagnosis and treatment are crucial for managing chronic respiratory diseases effectively. Early detection allows for prompt intervention, preventing disease progression and improving patient outcomes. For example, early diagnosis of COPD enables the implementation of strategies to slow disease progression, such as smoking cessation and pulmonary rehabilitation.
Preventing Respiratory Illnesses
Preventing respiratory illnesses is a key component of public health. Several strategies can be implemented to reduce the incidence of respiratory diseases, including:
- Promoting smoking cessation: Smoking is a major risk factor for COPD and other respiratory diseases. Public health campaigns and smoking cessation programs are crucial in reducing smoking prevalence.
- Improving air quality: Air pollution is another significant contributor to respiratory illnesses. Policies aimed at reducing air pollution, such as promoting cleaner transportation and industrial emissions control, can significantly impact public health.
- Promoting healthy respiratory habits: Encouraging healthy respiratory habits, such as regular exercise, maintaining a healthy weight, and avoiding exposure to allergens and irritants, can help prevent respiratory illnesses.
Promoting Healthy Respiratory Habits
Public health initiatives should emphasize the importance of healthy respiratory habits to reduce the risk of developing respiratory illnesses. These habits include:
- Regular exercise: Regular physical activity strengthens the respiratory system and improves lung function, reducing the risk of developing respiratory diseases.
- Maintaining a healthy weight: Obesity can exacerbate respiratory conditions, making it crucial to maintain a healthy weight.
- Avoiding exposure to allergens and irritants: Exposure to allergens and irritants can trigger asthma attacks and worsen COPD symptoms. Measures to minimize exposure, such as avoiding smoke, dust, and pet dander, can improve respiratory health.
Historical Perspective on Ipratropium
Ipratropium bromide, a synthetic anticholinergic drug, has played a pivotal role in the management of respiratory diseases since its introduction in the 1980s. Its development and subsequent impact on patient care represent a significant milestone in the history of respiratory medicine.
Development and Discovery of Ipratropium
The journey of ipratropium began with the exploration of the anticholinergic properties of atropine, a naturally occurring alkaloid. Atropine, extracted from the deadly nightshade plant, had been used for centuries to treat a variety of ailments, including respiratory conditions. However, its systemic effects, including cardiovascular side effects, limited its use.
- In the 1960s, researchers began investigating synthetic analogs of atropine with the goal of developing drugs with more selective and localized actions. This led to the discovery of ipratropium, a compound with a similar structure to atropine but with a higher affinity for muscarinic receptors in the airways.
- Ipratropium was first synthesized by researchers at Boehringer Ingelheim in the early 1970s. It was initially tested for its potential to treat asthma and other respiratory diseases.
- Clinical trials in the 1980s demonstrated the efficacy of ipratropium in improving lung function and reducing symptoms in patients with chronic obstructive pulmonary disease (COPD) and asthma.
Impact of Ipratropium on Respiratory Disease Management
The introduction of ipratropium marked a significant shift in the management of respiratory diseases. Prior to ipratropium, treatment options for COPD and asthma were limited. Bronchodilators like epinephrine and isoproterenol were available, but they had a short duration of action and could cause significant side effects.
- Ipratropium’s long-acting bronchodilating properties and its relatively low incidence of systemic side effects made it a valuable addition to the therapeutic arsenal.
- Ipratropium helped improve the quality of life for millions of patients suffering from COPD and asthma. It enabled them to breathe easier, engage in physical activity, and lead more fulfilling lives.
Evolution of Ipratropium Formulations and Therapeutic Strategies
Since its initial introduction, ipratropium has undergone significant advancements in terms of formulation and therapeutic strategies.
- Initially, ipratropium was available as an aerosol solution for inhalation.
- Later, newer formulations were developed, including dry powder inhalers (DPIs) and nebulized solutions. These advancements made it easier for patients to administer ipratropium and improve adherence to treatment.
- Ipratropium has also been combined with other medications, such as albuterol, a short-acting beta-agonist, to provide synergistic bronchodilation.
- The development of combination therapies has further enhanced the effectiveness of ipratropium in managing respiratory diseases.
Ipratropium stands as a valuable tool in the arsenal of respiratory disease management. Its ability to relax airway muscles, alleviate symptoms, and improve lung function makes it an essential medication for many individuals. Understanding its mechanism of action, potential side effects, and appropriate usage is crucial for maximizing its benefits and ensuring patient safety.
Ipratropium is a medication used to treat respiratory conditions like asthma and chronic obstructive pulmonary disease (COPD). It works by relaxing the muscles in the airways, making it easier to breathe. While ipratropium is helpful for managing these conditions, it’s important to remember that it’s not a cure. For patients with multiple sclerosis, another medication, avonex , might be prescribed.
Avonex is a treatment that helps to slow the progression of the disease. Both medications are crucial for managing their respective conditions, providing relief and improving quality of life for patients.