Prazosin, a medication known for its alpha-blocking properties, has played a significant role in the treatment of various medical conditions. From its discovery as a potential antihypertensive agent to its current applications in managing conditions like benign prostatic hyperplasia and post-traumatic stress disorder, prazosin’s journey reflects the evolving landscape of medicine.
This comprehensive guide delves into the intricate workings of prazosin, exploring its mechanism of action, therapeutic uses, pharmacokinetic profile, potential adverse effects, and safety considerations. We will also examine the clinical applications of prazosin in different medical specialties and discuss ongoing research efforts exploring its potential for new therapeutic applications.
Prazosin
Prazosin is a medication primarily used to treat high blood pressure (hypertension) and to improve urinary symptoms in men with an enlarged prostate (benign prostatic hyperplasia, BPH). It belongs to a class of drugs called alpha-blockers.
Overview and History
Prazosin is a potent alpha-adrenergic receptor antagonist. This means it blocks the effects of norepinephrine and epinephrine, hormones that cause blood vessels to constrict. By blocking these receptors, prazosin relaxes blood vessels, leading to a decrease in blood pressure.
The discovery of prazosin can be traced back to the 1960s, when researchers at the pharmaceutical company Pfizer were investigating new drugs for the treatment of hypertension. They identified a compound, code-named “SQ 6539,” which showed promise in lowering blood pressure. Further research led to the development of prazosin, which was first approved for use in the United States in 1975.
Initially, prazosin was primarily used to treat hypertension. However, it was later found to be effective in improving urinary symptoms associated with BPH. This discovery led to the widespread use of prazosin for both conditions.
Chemical Properties
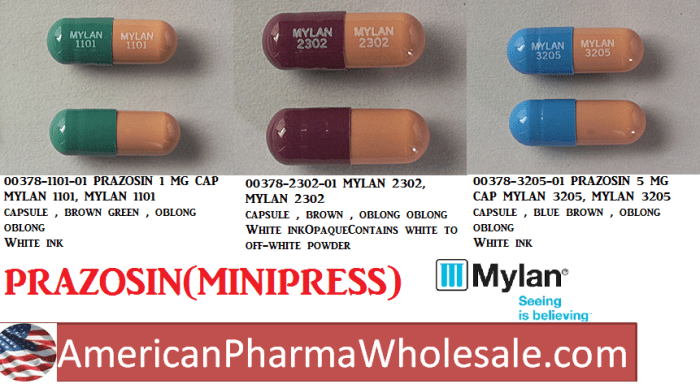
Prazosin is a white to off-white crystalline powder that is practically insoluble in water. Its chemical formula is C19H21N5O4 and its molecular weight is 383.4 g/mol.
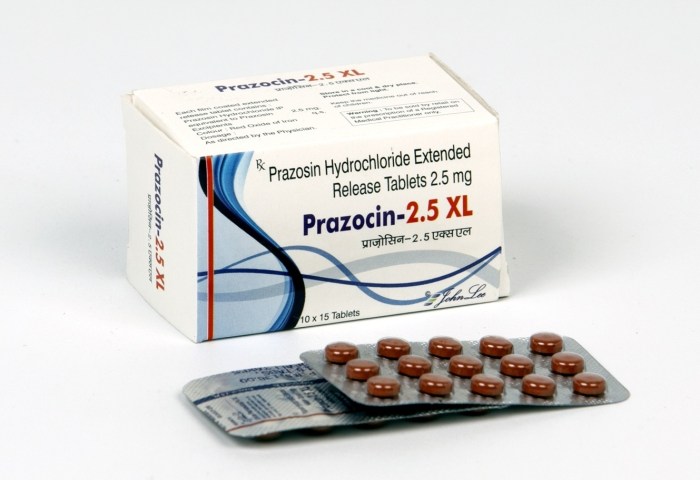
Prazosin is available in various forms, including tablets, capsules, and oral solutions.
The chemical structure of prazosin is characterized by a quinazoline ring system, which is responsible for its pharmacological activity.
Mechanism of Action
Prazosin’s primary mechanism of action revolves around its selective antagonism of alpha-1 adrenergic receptors. These receptors are found in various tissues throughout the body, including the smooth muscle of blood vessels, the prostate, and the bladder.
Prazosin’s interaction with alpha-1 adrenergic receptors leads to a blockade of the effects of norepinephrine and epinephrine, the primary neurotransmitters responsible for activating these receptors. This blockade results in relaxation of smooth muscle, particularly in the blood vessels, leading to vasodilation and a decrease in blood pressure.
Effects of Blocking Alpha-1 Adrenergic Receptors
Blocking alpha-1 adrenergic receptors has several physiological effects:
- Vasodilation: Prazosin’s blockade of alpha-1 receptors in blood vessels leads to relaxation of smooth muscle, resulting in vasodilation. This vasodilation reduces peripheral vascular resistance, lowering blood pressure.
- Improved Urinary Flow: In men with benign prostatic hyperplasia (BPH), prazosin’s blockade of alpha-1 receptors in the prostate relaxes the smooth muscle, improving urinary flow and reducing symptoms like difficulty urinating and frequent urination.
- Reduced Postural Hypotension: Prazosin’s vasodilating effects can reduce postural hypotension, a condition characterized by a sudden drop in blood pressure upon standing. This effect is due to the increased blood flow and reduced peripheral vascular resistance caused by prazosin.
Comparison with Other Alpha-Blockers
Prazosin is classified as a selective alpha-1 blocker, meaning it preferentially binds to and blocks alpha-1 receptors over alpha-2 receptors. Other alpha-blockers, such as doxazosin and terazosin, also belong to this class of drugs. However, there are some differences in their selectivity and pharmacokinetic profiles. For instance, prazosin has a shorter half-life compared to doxazosin and terazosin, leading to a shorter duration of action.
Prazosin’s selective antagonism of alpha-1 adrenergic receptors, particularly in blood vessels, leads to vasodilation and a reduction in blood pressure. This effect is the primary mechanism by which prazosin treats hypertension.
Therapeutic Uses

Prazosin is a medication primarily used to treat hypertension (high blood pressure) and benign prostatic hyperplasia (BPH). It belongs to a class of drugs known as alpha-blockers, which work by relaxing the muscles in the blood vessels and prostate.
Hypertension
Prazosin effectively reduces blood pressure by relaxing the muscles in the blood vessels, allowing blood to flow more easily. This reduces the workload on the heart and helps to lower blood pressure. Prazosin is often prescribed as part of a multi-drug regimen to manage hypertension, particularly in individuals with resistant hypertension, which is high blood pressure that is not adequately controlled by other medications.
Benign Prostatic Hyperplasia (BPH)
Prazosin is also used to treat BPH, a condition that causes the prostate gland to enlarge, leading to urinary symptoms such as difficulty urinating, weak urine stream, and frequent urination. Prazosin works by relaxing the muscles in the prostate gland, making it easier to urinate.
Other Uses, Prazosin
Prazosin has also been studied for its potential use in treating other conditions, such as:
- Post-traumatic stress disorder (PTSD): Prazosin has been shown to reduce nightmares and improve sleep quality in individuals with PTSD. It’s believed that prazosin may work by blocking the effects of norepinephrine, a neurotransmitter that is involved in the stress response.
- Raynaud’s phenomenon: Prazosin may help to improve blood flow to the hands and feet in people with Raynaud’s phenomenon, a condition that causes the blood vessels in the extremities to constrict in response to cold or stress.
Pharmacokinetics and Metabolism
Prazosin’s pharmacokinetic profile dictates how the drug is absorbed, distributed, metabolized, and eliminated from the body. Understanding these processes is crucial for optimizing therapeutic efficacy and minimizing potential adverse effects.
Absorption
Prazosin is well-absorbed after oral administration, with peak plasma concentrations typically achieved within 1-3 hours. However, the absolute bioavailability of prazosin is estimated to be around 50%, indicating that a portion of the drug is not absorbed or is metabolized during the first pass through the liver. The rate and extent of absorption can be influenced by the presence of food, with higher concentrations observed when prazosin is taken on an empty stomach.
Distribution
Prazosin is extensively distributed throughout the body, with a high volume of distribution. This suggests that the drug readily distributes into tissues and organs, including the heart, blood vessels, and kidneys. The distribution of prazosin is influenced by its high affinity for alpha-1 adrenergic receptors, which are found in various tissues.
Metabolism
Prazosin undergoes extensive hepatic metabolism, primarily through the cytochrome P450 (CYP) enzyme system, specifically CYP3A4. The major metabolites of prazosin are inactive and are excreted in the urine.
Excretion
Prazosin is eliminated from the body primarily through the kidneys, with a half-life of approximately 2-3 hours. This means that it takes about 2-3 hours for the plasma concentration of prazosin to decrease by half. However, the elimination half-life can be prolonged in patients with impaired renal function.
Factors Influencing Pharmacokinetic Profile
Several factors can influence prazosin’s pharmacokinetic profile, including:
- Age: Elderly patients may have reduced hepatic and renal function, leading to slower metabolism and elimination of prazosin, potentially increasing the risk of adverse effects.
- Liver disease: Patients with liver disease may experience impaired metabolism of prazosin, leading to higher and prolonged plasma concentrations, increasing the risk of adverse effects.
- Renal disease: Patients with renal disease may experience impaired elimination of prazosin, leading to higher and prolonged plasma concentrations, increasing the risk of adverse effects.
- Drug interactions: Certain drugs, such as strong CYP3A4 inhibitors, can inhibit the metabolism of prazosin, leading to higher and prolonged plasma concentrations, increasing the risk of adverse effects.
- Food: The presence of food in the stomach can delay the absorption of prazosin, leading to lower peak plasma concentrations and a slower onset of action.
Dosage and Frequency
The typical starting dose of prazosin is 1 mg orally once daily at bedtime. The dose can be gradually increased in increments of 1-2 mg every 3-7 days, depending on the individual’s response and tolerance. The maximum daily dose is typically 20 mg.
Prazosin is generally well-tolerated at therapeutic doses, but it is important to monitor patients for potential adverse effects, such as orthostatic hypotension, dizziness, and drowsiness.
Prazosin stands as a testament to the ongoing advancements in medical science, offering a valuable tool for managing a range of conditions. By understanding its multifaceted nature, healthcare professionals and patients alike can leverage its therapeutic potential while navigating potential risks and optimizing treatment outcomes.
Prazosin is a medication often used to treat high blood pressure, but it can also be effective in managing nightmares associated with post-traumatic stress disorder (PTSD). While prazosin focuses on the brain, a different type of medication like salbutamol is used for respiratory issues. Salbutamol, a bronchodilator, helps open up airways and is commonly used for conditions like asthma. You can learn more about the specific uses of salbutamol here.
Prazosin, on the other hand, works to block certain receptors in the brain, ultimately reducing the intensity of nightmares.