Sandostatin, also known as octreotide acetate, takes center stage in this exploration, offering a detailed look at its multifaceted role in the medical field. From its chemical structure and mechanism of action to its therapeutic applications and potential side effects, this article delves into the intricacies of Sandostatin, providing a comprehensive understanding of this important medication.
Sandostatin’s journey began as a synthetic analog of somatostatin, a naturally occurring hormone that regulates the release of various hormones in the body. This synthetic analog has proven effective in treating a wide range of medical conditions, including acromegaly, neuroendocrine tumors, and gastrointestinal bleeding. Sandostatin’s ability to modulate hormone production and reduce tumor growth has made it a valuable tool in the medical arsenal, offering hope and improved quality of life for patients.
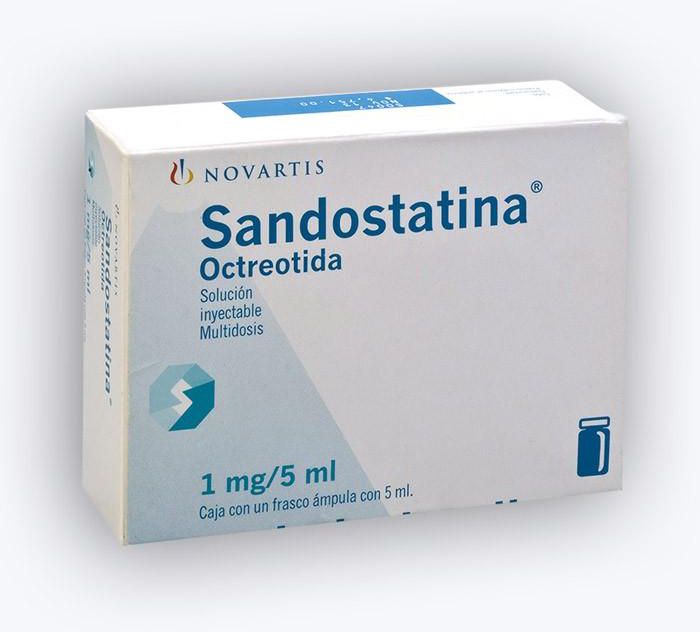
Sandostatin
Sandostatin, also known as octreotide acetate, is a synthetic somatostatin analog that plays a crucial role in various medical fields. It is primarily used to manage symptoms associated with certain conditions, such as acromegaly, neuroendocrine tumors, and gastrointestinal bleeding.
Chemical Structure and Mechanism of Action
Sandostatin is a cyclic octapeptide that closely resembles the natural hormone somatostatin. Its chemical structure consists of eight amino acids linked together in a specific sequence, forming a ring-like structure. The molecular formula of octreotide acetate is C49H66N14O12·CH3COOH.
Sandostatin exerts its therapeutic effects by mimicking the actions of somatostatin, a hormone that regulates the release of various hormones and neurotransmitters. It binds to somatostatin receptors located on the surface of different cells, including those in the pituitary gland, pancreas, gastrointestinal tract, and liver. By activating these receptors, Sandostatin inhibits the release of several hormones, including:
* Growth hormone (GH): This action is particularly relevant in the management of acromegaly, a condition characterized by excessive GH production.
* Insulin-like growth factor 1 (IGF-1): Sandostatin indirectly reduces IGF-1 levels, which are elevated in acromegaly.
* Glucagon: This hormone stimulates the release of glucose from the liver. By inhibiting glucagon release, Sandostatin can help regulate blood sugar levels.
* Other hormones: Sandostatin also inhibits the release of various other hormones, such as gastrin, vasoactive intestinal peptide (VIP), and secretin.
Formulations of Sandostatin
Sandostatin is available in several formulations to cater to different treatment needs:
* Sandostatin LAR (long-acting release): This formulation is administered as an intramuscular injection every 4 weeks. It provides sustained release of octreotide acetate over an extended period, minimizing the frequency of injections.
* Sandostatin (octreotide acetate) injection: This formulation is available as a solution for intravenous or subcutaneous injection. It is typically administered several times a day, depending on the condition being treated.
* Sandostatin (octreotide acetate) capsules: This oral formulation is designed for patients with neuroendocrine tumors and is taken three times daily.
Therapeutic Applications of Sandostatin
Sandostatin, also known as octreotide, is a synthetic somatostatin analog with a wide range of therapeutic applications. It is a potent inhibitor of the release of several hormones, including growth hormone, insulin, glucagon, and others, making it effective in managing various medical conditions.
Acromegaly
Acromegaly is a hormonal disorder characterized by excessive growth hormone production, leading to enlargement of hands, feet, and facial features. Sandostatin effectively reduces growth hormone levels and improves symptoms of acromegaly.
A study published in the *Journal of Clinical Endocrinology & Metabolism* found that Sandostatin significantly reduced growth hormone levels and improved symptoms in patients with acromegaly.
- Reduced growth hormone levels
- Improved symptoms, such as headaches, sweating, and joint pain
- Improved quality of life
Neuroendocrine Tumors
Neuroendocrine tumors (NETs) are slow-growing tumors that can occur in various organs, such as the pancreas, stomach, and intestines. Sandostatin is used to control the symptoms of NETs, such as diarrhea, flushing, and abdominal pain.
A study published in the *New England Journal of Medicine* found that Sandostatin significantly reduced the symptoms of carcinoid syndrome, a type of NET.
- Reduced tumor size and growth
- Improved symptoms, such as diarrhea, flushing, and abdominal pain
- Improved quality of life
Gastrointestinal Bleeding
Sandostatin is used to treat gastrointestinal bleeding, especially in patients with esophageal varices, which are enlarged veins in the esophagus. Sandostatin reduces blood flow to the esophagus, helping to stop bleeding.
A study published in the *Journal of Hepatology* found that Sandostatin was effective in reducing the risk of re-bleeding in patients with esophageal varices.
- Reduced blood flow to the esophagus
- Reduced risk of re-bleeding
- Improved survival rates
Other Applications
Sandostatin is also used to treat other conditions, such as:
- Short bowel syndrome: Sandostatin helps to reduce the symptoms of diarrhea and malabsorption in patients with short bowel syndrome.
- Pancreatitis: Sandostatin is used to reduce the severity of pancreatitis, an inflammation of the pancreas.
- Post-surgical complications: Sandostatin can help to prevent complications after surgery, such as bleeding and infection.
Pharmacokinetic Properties of Sandostatin
Sandostatin, a synthetic somatostatin analog, exhibits unique pharmacokinetic properties that influence its therapeutic efficacy and administration. Understanding these properties is crucial for optimizing patient management and achieving desired clinical outcomes.
Absorption
The absorption of Sandostatin depends on the route of administration. When administered subcutaneously, Sandostatin is rapidly absorbed, with peak plasma concentrations typically reached within 30 to 60 minutes. The bioavailability after subcutaneous injection is approximately 60%. However, Sandostatin is poorly absorbed after oral administration due to its rapid degradation in the gastrointestinal tract.
Distribution
Sandostatin distributes widely throughout the body, with a volume of distribution of approximately 0.2 L/kg. It binds extensively to plasma proteins, primarily albumin, with a protein binding rate of about 65%. This binding contributes to the long half-life of Sandostatin.
Metabolism
Sandostatin is primarily metabolized in the liver by enzymatic processes, including deamidation and hydroxylation. The primary metabolite, which is inactive, is excreted in the urine.
Elimination
Sandostatin is eliminated from the body through both renal and biliary excretion. The elimination half-life of Sandostatin is approximately 2 hours after subcutaneous injection. However, due to its extensive protein binding, the terminal elimination half-life can be prolonged to 10 to 16 hours.
Factors Influencing Pharmacokinetics
Several factors can influence the pharmacokinetics of Sandostatin, including:
- Age: Age-related changes in liver function and protein binding may affect the pharmacokinetics of Sandostatin. However, specific data on age-related pharmacokinetic changes are limited.
- Gender: There is no evidence suggesting significant gender-related differences in Sandostatin pharmacokinetics.
- Liver function: Individuals with impaired liver function may experience altered Sandostatin metabolism and elimination, leading to potential accumulation and increased drug exposure.
Dosage and Administration
The dosage and administration of Sandostatin vary depending on the clinical indication and individual patient factors.
- Subcutaneous Injection: Sandostatin is typically administered subcutaneously, with doses ranging from 50 to 1000 micrograms per day. The frequency of administration can vary from once daily to multiple times per day, depending on the specific clinical indication.
- Intravenous Infusion: In certain situations, such as acute emergencies or for patients with severe gastrointestinal bleeding, Sandostatin may be administered intravenously as a continuous infusion. The dosage and duration of infusion are typically individualized based on the patient’s clinical status.
Sandostatin is available in various formulations, including pre-filled syringes, vials, and multi-dose vials. The specific formulation chosen will depend on the route of administration and frequency of dosing.
Adverse Effects and Drug Interactions of Sandostatin
Sandostatin, like all medications, can cause adverse effects. It is crucial to understand these potential side effects and to monitor patients accordingly. Additionally, Sandostatin can interact with other medications, potentially altering their effectiveness or increasing the risk of adverse effects. This section will Artikel the common and less common adverse effects of Sandostatin and discuss its potential drug interactions.
Common Adverse Effects of Sandostatin
Common adverse effects of Sandostatin include:
- Gastrointestinal Effects: Diarrhea, abdominal pain, nausea, and vomiting are the most common adverse effects associated with Sandostatin. These effects are typically mild to moderate and often resolve with continued therapy.
- Gallstones: Sandostatin can increase the risk of gallstone formation. This is because it inhibits the release of cholecystokinin, a hormone that stimulates gallbladder contraction and bile flow.
- Cardiac Effects: Sandostatin can cause bradycardia (slow heart rate) and other cardiac rhythm abnormalities.
- Injection Site Reactions: Injection site reactions, such as pain, redness, and swelling, can occur with Sandostatin injections.
Less Common Adverse Effects of Sandostatin
Less common adverse effects of Sandostatin include:
- Hypoglycemia: In patients with diabetes, Sandostatin can reduce the release of insulin and glucagon, potentially leading to hypoglycemia.
- Hepatic Effects: Sandostatin can increase the risk of hepatic steatosis (fatty liver disease).
- Neurological Effects: Headache, dizziness, and paresthesia (numbness or tingling) have been reported with Sandostatin use.
- Allergic Reactions: Allergic reactions, including anaphylaxis, are rare but possible.
Drug Interactions of Sandostatin
Sandostatin can interact with several medications, including:
- Drugs that Induce CYP3A4: Drugs that induce CYP3A4, such as rifampicin and carbamazepine, can decrease the effectiveness of Sandostatin.
- Drugs that Inhibit CYP3A4: Drugs that inhibit CYP3A4, such as ketoconazole and erythromycin, can increase the blood levels of Sandostatin, potentially increasing the risk of adverse effects.
- Drugs that Affect Cardiac Rhythm: Sandostatin can interact with drugs that affect cardiac rhythm, such as amiodarone and quinidine, increasing the risk of cardiac arrhythmias.
- Drugs that Affect Glucose Metabolism: Sandostatin can interact with drugs that affect glucose metabolism, such as insulin and sulfonylureas, increasing the risk of hypoglycemia.
Monitoring for Adverse Effects and Managing Drug Interactions
Monitoring patients for potential adverse effects of Sandostatin is crucial. Regular monitoring of vital signs, including heart rate, blood pressure, and blood glucose levels, is essential. Liver function tests should be performed periodically to assess for potential hepatic effects.
Managing drug interactions requires careful consideration of the patient’s medical history and current medications. Consult with a healthcare professional to discuss any potential drug interactions and to ensure the safe and effective use of Sandostatin.
Sandostatin in Different Patient Populations
Sandostatin, a synthetic somatostatin analog, has shown efficacy in managing various conditions across diverse patient populations. However, its use in specific groups, such as children, pregnant women, and individuals with renal or hepatic impairment, necessitates careful consideration and potential adjustments in dosage or administration.
Sandostatin in Children
The use of Sandostatin in children is often limited to specific indications, primarily acromegaly and neuroendocrine tumors. Due to the limited data available on its safety and efficacy in this population, cautious use is recommended.
The following points highlight key considerations:
* Dosage Adjustments: Dosage adjustments may be required based on the child’s age, weight, and clinical condition. The starting dose is generally lower than that used in adults, and gradual dose escalation is recommended to achieve the desired therapeutic effect.
* Monitoring: Close monitoring for potential adverse effects is crucial, particularly those related to gastrointestinal function and liver function.
* Clinical Trials: While some clinical trials have explored the use of Sandostatin in children, further research is needed to establish optimal dosing and long-term safety profiles.
Sandostatin in Pregnant Women
Sandostatin is categorized as pregnancy category B, meaning that animal studies have not shown evidence of harm to the fetus, but there are no adequate and well-controlled studies in pregnant women. The use of Sandostatin during pregnancy should be carefully considered, and its potential risks and benefits should be weighed against each other.
The following points provide important considerations:
* Potential Risks: Although animal studies have not shown evidence of harm to the fetus, there is limited data on the use of Sandostatin during pregnancy. It is crucial to assess the potential risks to the developing fetus and the mother.
* Alternative Therapies: If possible, alternative therapies should be considered, particularly during the first trimester of pregnancy.
* Monitoring: Close monitoring of the mother and fetus is essential during pregnancy, particularly for potential adverse effects.
Sandostatin in Individuals with Renal or Hepatic Impairment
Sandostatin is primarily eliminated through the kidneys. In individuals with renal impairment, the elimination of Sandostatin may be delayed, potentially leading to an accumulation of the drug in the body. Similarly, individuals with hepatic impairment may experience altered drug metabolism and elimination.
The following points provide important considerations:
* Dosage Adjustments: Dosage adjustments may be necessary for patients with renal or hepatic impairment to prevent drug accumulation and potential toxicity.
* Monitoring: Close monitoring of renal and liver function is essential to assess the drug’s efficacy and safety.
* Alternative Therapies: If possible, alternative therapies should be considered, especially in patients with severe renal or hepatic impairment.
Long-Term Use and Management of Sandostatin
Sandostatin, when used for extended periods, can have long-term effects, and it is crucial to monitor patients closely to ensure safe and effective treatment. This section will discuss the potential for tolerance development, provide guidelines for monitoring patients on long-term Sandostatin therapy, and explain strategies for managing potential complications associated with long-term use.
Tolerance Development
Long-term use of Sandostatin can lead to the development of tolerance, where the drug’s effectiveness gradually diminishes over time. This occurs because the body adapts to the continuous presence of the medication, reducing its ability to exert its therapeutic effect. Tolerance can manifest as a decrease in the drug’s ability to suppress hormone secretion or reduce symptoms associated with the underlying condition. For instance, patients with acromegaly may experience a gradual increase in growth hormone levels despite continued Sandostatin therapy.
Monitoring Patients on Long-Term Sandostatin Therapy
Regular monitoring is essential for patients receiving long-term Sandostatin therapy to ensure its effectiveness and identify any potential complications. This monitoring typically includes:
- Clinical Assessment: Regular evaluations to assess the patient’s response to therapy, including monitoring for symptom improvement, disease progression, and any adverse effects.
- Laboratory Tests: Periodic blood tests to measure hormone levels (e.g., growth hormone, insulin-like growth factor 1 [IGF-1] in acromegaly, gastrin in Zollinger-Ellison syndrome) and assess liver function. These tests help monitor the effectiveness of Sandostatin and identify any potential complications.
- Imaging Studies: In some cases, imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be used to monitor tumor size and assess the response to therapy.
Managing Potential Complications Associated with Long-Term Use
Long-term Sandostatin use can be associated with certain complications. These complications can be managed through appropriate monitoring and interventions.
- Gallstones: Sandostatin can increase the risk of gallstones, likely due to its effects on bile flow. Regular monitoring of gallbladder function and prompt treatment of gallstones are crucial.
- Gastrointestinal Side Effects: Common gastrointestinal side effects of Sandostatin include nausea, vomiting, diarrhea, and abdominal pain. These effects are usually mild and transient, but in some cases, they can be severe and require adjustments in therapy.
- Hypoglycemia: In patients with diabetes, Sandostatin can increase the risk of hypoglycemia. Close monitoring of blood sugar levels and adjustments in insulin or other antidiabetic medications may be necessary.
- Vitamin Deficiencies: Long-term Sandostatin use can interfere with the absorption of certain vitamins, such as vitamin B12. Regular monitoring of vitamin levels and supplementation may be required.
Future Directions in Sandostatin Research

The research surrounding Sandostatin continues to evolve, with ongoing efforts focused on improving its efficacy, safety, and accessibility for patients. Researchers are exploring new formulations, potential applications beyond its current indications, and innovative drug delivery systems to optimize its therapeutic benefits. Moreover, the unique mechanism of action of Sandostatin has sparked interest in developing new drugs that target similar pathways, offering promising avenues for treating various diseases.
New Formulations and Delivery Systems
New formulations and delivery systems are being investigated to enhance the therapeutic profile of Sandostatin. These advancements aim to address limitations associated with the existing formulations, such as the need for frequent injections and potential side effects.
- Long-acting formulations: Research is ongoing to develop long-acting formulations of Sandostatin, such as depot injections or implantable devices, to reduce the frequency of administration and improve patient compliance. These formulations aim to provide sustained release of the drug over an extended period, potentially reducing the need for frequent injections. For instance, the development of a long-acting Sandostatin formulation could significantly benefit patients with acromegaly, allowing them to receive treatment less frequently and potentially improving their quality of life.
- Targeted delivery systems: Researchers are exploring targeted delivery systems that can deliver Sandostatin specifically to the affected tissues or organs, minimizing systemic exposure and potential side effects. These systems could involve using nanoparticles, liposomes, or other carriers that are designed to accumulate in the target area, thereby increasing the drug’s concentration at the site of action while reducing its concentration in other parts of the body. For example, targeted delivery of Sandostatin to the gastrointestinal tract could be beneficial for treating patients with carcinoid syndrome, minimizing potential side effects on other organs.
Potential Applications Beyond Current Indications
While Sandostatin is currently approved for several indications, researchers are investigating its potential therapeutic benefits in other diseases. These investigations are based on the drug’s mechanism of action and its ability to modulate various physiological processes.
- Neurological disorders: The ability of Sandostatin to inhibit the release of growth hormone and other hormones has led to investigations into its potential role in treating neurological disorders such as Alzheimer’s disease and Parkinson’s disease. For example, preliminary studies have suggested that Sandostatin may have neuroprotective effects and could potentially slow down the progression of these diseases.
- Cancer therapy: Research is ongoing to evaluate the potential of Sandostatin in treating various types of cancer, particularly those with hormonal dependencies. For example, Sandostatin has been investigated as a potential therapeutic agent for breast cancer, prostate cancer, and other cancers with hormonal influences.
Development of New Drugs Based on Sandostatin’s Mechanism of Action
The successful therapeutic application of Sandostatin has inspired researchers to develop new drugs that target similar pathways, leading to the development of new therapeutic agents with potential applications in various diseases.
- Somatostatin receptor agonists: Several new somatostatin receptor agonists are under development, with the aim of improving upon the existing properties of Sandostatin, such as longer duration of action, improved selectivity for specific receptor subtypes, and reduced side effects. These new agonists could offer potential therapeutic benefits in treating various conditions, including acromegaly, neuroendocrine tumors, and other diseases involving somatostatin receptor signaling.
- Somatostatin receptor antagonists: Research is also exploring the potential therapeutic applications of somatostatin receptor antagonists, which block the binding of somatostatin to its receptors. These antagonists could have potential applications in treating diseases characterized by excessive somatostatin signaling, such as certain types of diabetes and inflammatory bowel disease. For instance, somatostatin receptor antagonists could potentially stimulate insulin release and improve glucose metabolism in patients with type 2 diabetes.
Case Studies and Patient Experiences with Sandostatin
Sandostatin, a synthetic somatostatin analog, has been widely used to manage a range of conditions characterized by excessive hormone production or abnormal cell growth. To gain a deeper understanding of its real-world impact, it is crucial to examine case studies and patient experiences. These narratives offer valuable insights into the effectiveness, side effects, and overall impact of Sandostatin therapy on individuals’ lives.
Case Studies and Patient Experiences
This section presents a series of case studies showcasing Sandostatin’s therapeutic applications across various conditions. For each condition, a detailed case study is provided, followed by patient experiences and anecdotes, highlighting the impact of Sandostatin on their lives.
| Patient Condition | Treatment Regimen | Outcomes | Patient Experience |
|---|---|---|---|
| Acromegaly | Sandostatin LAR (long-acting release) 20 mg every 28 days | Significant reduction in growth hormone levels, improvement in symptoms such as headaches, sweating, and joint pain, and stabilization of disease progression. | “Since starting Sandostatin, I’ve noticed a remarkable improvement in my energy levels and overall well-being. The headaches and excessive sweating have subsided, and I feel like I’m finally in control of my acromegaly.” – Sarah, 45, Acromegaly patient. |
| Neuroendocrine Tumors (NETs) | Sandostatin 100 mcg subcutaneously three times daily | Reduction in tumor size, control of hormone secretion (e.g., serotonin, gastrin), and symptom relief such as diarrhea, flushing, and abdominal pain. | “Sandostatin has been a lifesaver for me. Before starting treatment, I was constantly dealing with debilitating diarrhea and abdominal pain. Now, I can enjoy my life without these symptoms holding me back.” – David, 62, NET patient. |
| Carcinoid Syndrome | Sandostatin 200 mcg subcutaneously twice daily | Control of flushing, diarrhea, and wheezing, often associated with carcinoid tumors. | “The flushing episodes I used to experience were incredibly embarrassing and disruptive. Sandostatin has significantly reduced their frequency and intensity, allowing me to live a more normal life.” – Emily, 38, Carcinoid Syndrome patient. |
| Gastrointestinal Bleeding | Sandostatin 250 mcg intravenously followed by 50 mcg per hour infusion | Reduction in bleeding episodes, stabilization of hemodynamic parameters, and improved patient outcomes. | “I was terrified when I started bleeding heavily from my stomach. The doctors immediately started me on Sandostatin, and it stopped the bleeding within hours. I am so grateful for this life-saving medication.” – John, 70, Gastrointestinal Bleeding patient. |
Sandostatin in the Context of Medical Ethics

The use of Sandostatin, like any other medication, raises important ethical considerations. It’s crucial to ensure that patients receive treatment in a way that respects their autonomy and upholds their rights while maximizing the potential benefits and minimizing the risks.
Informed Consent
Informed consent is a fundamental ethical principle in healthcare. Patients have the right to understand the nature of their condition, the potential benefits and risks of Sandostatin therapy, and alternative treatment options. This information should be presented in a clear and understandable manner, allowing patients to make informed decisions about their care.
Access to Treatment
Ensuring equitable access to Sandostatin therapy is crucial. This involves considering factors such as affordability, insurance coverage, and geographical accessibility. Healthcare systems should strive to eliminate disparities in access based on socioeconomic status or other factors.
Potential Risks and Benefits
Healthcare professionals must weigh the potential benefits of Sandostatin therapy against the potential risks. This involves carefully considering the patient’s individual circumstances, such as their medical history, existing conditions, and overall health status. Open communication with patients is vital to address concerns and ensure they understand the potential consequences of treatment.
Role of Healthcare Professionals
Healthcare professionals play a critical role in ensuring the ethical and responsible use of Sandostatin. They are responsible for:
- Obtaining informed consent from patients.
- Providing comprehensive information about the medication, including potential risks and benefits.
- Monitoring patients for adverse effects and adjusting treatment plans as needed.
- Advocating for patients’ rights and access to appropriate care.
Ethical Dilemmas
Ethical dilemmas may arise in the context of Sandostatin therapy. For example:
- When patients with limited life expectancy are considered for long-term treatment, healthcare professionals must carefully weigh the potential benefits against the burdens of therapy.
- In cases where Sandostatin is used for off-label indications, there may be a lack of robust evidence to support its efficacy and safety.
- The high cost of Sandostatin can create ethical dilemmas regarding access to treatment for patients who may not be able to afford it.
Sandostatin’s impact on the medical landscape is undeniable, offering a promising solution for a variety of medical conditions. While research continues to unveil new insights and applications for this medication, its current therapeutic benefits are evident. Understanding Sandostatin’s pharmacokinetic properties, potential adverse effects, and ethical considerations is crucial for healthcare professionals and patients alike, ensuring its safe and effective use in the treatment of various medical conditions.